The effects of sugar on gut microbiome
Do you find yourself indulging in sugary snacks and processed foods often? But do your trillions of inhabitants in your gut agree?
In today’s modern world, sugar has become an inescapable part of our lives. From processed foods to sweetened beverages, we consume sugar in various forms daily, often without realizing it. This abnormal consumption of sugar not only impacts our overall health but also has a significant effect on our gut microbiome. The gut microbiome plays a crucial role in our well-being, and maintaining a balanced gut is essential for our overall health.
The role of sugar in our diets
Sugar, a simple carbohydrate, not only adds a sweet taste to our food and drinks but also provides our bodies with an essential source of energy. Our metabolism breaks down sugar into glucose, which is then used by our cells for various physiological processes. While being a natural component of many whole foods, such as fruits, it’s the added sugars found in processed foods and beverages that are of particular concern. Excessive sugar may have a negative impact on our health, leading to a range of issues such as obesity, type 2 diabetes, and cardiovascular disease. It is crucial to be mindful of our sugar intake and make informed dietary choices to maintain a healthy intestinal ecology and overall well-being.
Sugar | Dietary sources |
|---|---|
Glucose | Grains, honey |
Fructose | Fruits, vegetables, honey, agave nectar, and high fructose corn syrup |
Sucrose | Table sugar, sugarcane, sugar beets, and refined foods |
Lactose | Milk, yogurt, cheese, and other dairy products |
Maltose | Malt products, beer, and some processed foods |
High Fructose Corn Syrup | Soda, candy, refined foods, and sweetened beverages |
How does sugar affect the gut microbiome?
It is evident that high-sugar diets have increased significantly over the decades, primarily due to the widespread use of added sugars in processed foods and beverages. This excessive simple sugar intake not only contributes to obesity and other health issues but also has a substantial impact on our intestinal ecology. The human gut microbiota forms a complex community of microorganisms that reside in our intestines, playing a crucial role in digestion, immune function, and overall health. In the following sections, we will explore how sugary foods and beverages affects all human microbiomes and its implications on our well-being.
The link between sugar, dysbiosis, and health issues
Sugar serves as a fuel source for various gut bacteria, including both beneficial and harmful species. While some bacteria can utilize sugar to promote gut health, too much sugar can lead to the overgrowth of harmful bacteria and fungi, such as Candida albicans. This overgrowth can diminish the diversity of gut microbiota, which is crucial for maintaining a healthy gastrointestinal system and overall well-being.
Dysbiosis refers to an imbalance in the good bacteria and bad bacteria equilibrium. This imbalance can be triggered by high sugar consumption, leading to a cascade of health conditions. For example, certain pathogenic bacteria, such as Fusobacterium nucleatum, thrive on sugar and have been associated with colorectal cancer. Furthermore, the overgrowth of harmful bacteria can cause inflammation and damage to the gut lining, increasing the risk of cardiovascular disorders and other chronic diseases.
Each type of bacteria in the following table has been linked to a disease or a symptom:
Dysbiotic bacteria | Pathologic metabolite | Disease |
|---|---|---|
Candida albicans | Acetaldehyde | Oral and gastrointestinal candidiasis |
Fusobacterium nucleatum | Hydrogen sulfide | Colorectal cancer |
Clostridium difficile | Toxins A and B | Antibiotic-associated diarrhea, colitis |
Enterococcus faecalis | Biliverdin | Bacterial endocarditis, urinary tract infections |
Escherichia coli | Shiga toxin-producing strains | Gastroenteritis, urinary tract infections |
Bacteroides fragilis | Enterotoxins | Intra-abdominal infections, sepsis |
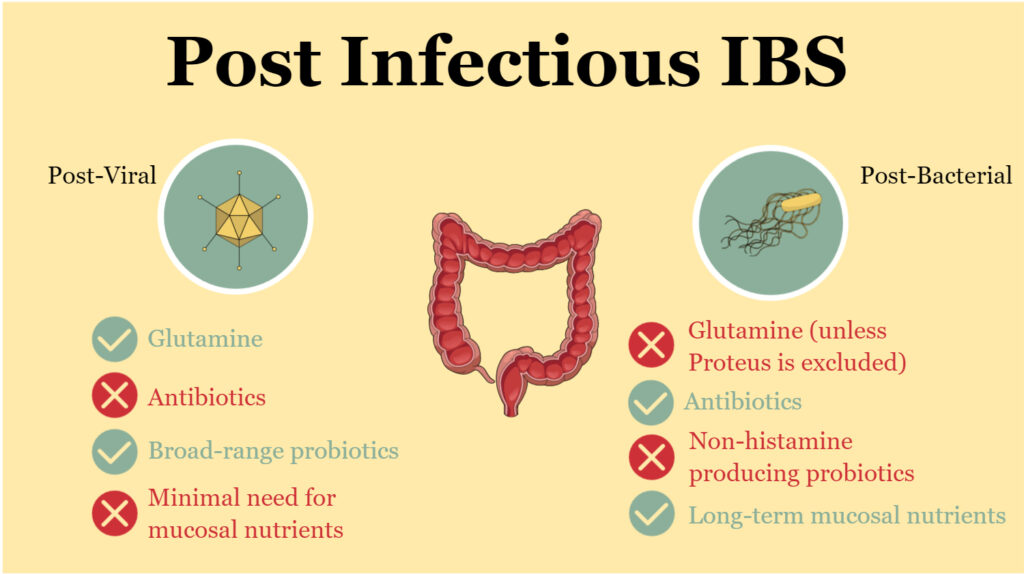
IBS: A hallmark syndrome of the "sugary" Western Diet
The effects of sugar on the gut microbiome are particularly relevant to individuals suffering from Irritable Bowel Syndrome (IBS), as the imbalances in gut bacteria can exacerbate the symptoms and further disrupt the delicate balance of the enteric nervous system. High sugar intake, especially from processed foods and beverages, can lead to the overgrowth of harmful bacteria such as Candida albicans and Klebsiella pneumoniae, which thrive on sugar and disrupt the overall microbial balance. In turn, this dysbiosis can cause increased fermentation in the gut, leading to bloating, flatulence, and other IBS symptoms.
Furthermore, the long-term effects of sugar consumption on the gut microbiome can promote dysbiotic states, which can have a significant impact on the enteric nervous system. This system, responsible for regulating gut function, may become dysregulated, leading to visceral hypersensitivity, a hallmark symptom of IBS. Visceral hypersensitivity is characterized by heightened sensitivity to pain, bloating, and changes in bowel habits. This increased sensitivity can be mediated by various hormones, such as serotonin and corticotropin-releasing factor, which play crucial roles in gut motility, inflammation, and stress responses.
Additionally, artificial sweeteners such as aspartame, saccharin, and sucralose, often used as sugar substitutes, can also negatively impact gut bacteria balance and contribute to dysbiosis. This can further exacerbate IBS symptoms and affect the enteric nervous system, perpetuating a vicious cycle of gut dysfunction, visceral hypersensitivity, and discomfort.
Symptom | Dysbiotic bacterium | Mechanism |
|---|---|---|
Bloating | Candida albicans | Fermentation of sugars |
Abdominal pain | Escherichia coli | Altered gut motility |
Diarrhea | Clostridium difficile | Toxin production |
Constipation | Bacteroides fragilis | Impaired short-chain fatty acid production |
Flatulence | Fusobacterium nucleatum | Hydrogen sulfide production |
Visceral hypersensitivity | Enterococcus faecalis | Gut inflammation, altered serotonin regulation |

Artificial sweeteners: Friend or foe?
Artificial sweeteners (or non-nutritive sweeteners) gained popularity in the latter half of the 20th century as a low-calorie alternative to sugar, appealing to those looking to reduce calorie intake or manage blood sugar levels. However, despite their low caloric content, recent studies (both in human and mouse studies) have shown that these sweeteners can negatively influence the human microbiome. Artificial sweeteners, such as aspartame, saccharin, and sucralose, can alter the balance of gut bacteria, potentially leading to dysbiosis and related health issues. One reason for this impact on the gut microbes is that these sweeteners are often consumed in liquid form, such as in diet sodas or sugar-free beverages, making them more readily available to gut bacteria. In light of these findings, it is essential to consider not only the caloric content of sweeteners but also their potential effects on gut health when making dietary choices.
Sweetener | Common food sources | Diseases studied |
|---|---|---|
Aspartame | Diet sodas, sugar-free gum, sugar substitutes | Metabolic syndrome, type 2 diabetes, gut dysbiosis |
Saccharin | Diet sodas, sugar substitutes, baked goods | Gut dysbiosis, glucose intolerance, weight gain |
Sucralose | Diet sodas, sugar substitutes, packaged foods | Gut dysbiosis, obesity, inflammatory bowel disease |
Acesulfame potassium (Ace-K) | Diet sodas, sugar-free desserts, sugar substitutes | Gut dysbiosis, metabolic disorders, obesity |
Neotame | Sugar substitutes, baked goods, beverages | Gut dysbiosis (limited data) |
Stevia (Rebaudioside A) | Sugar substitutes, beverages, packaged foods | Gut dysbiosis, glucose intolerance (limited data) |
Tips to reduce the effect of sugar on gut microbiota
Increase your fiber intake: Eat plenty of fruits, vegetables, whole grains, and legumes to promote a healthy gut environment.
Consume probiotics: Add fermented foods, such as yogurt, kefir, kimchi, and sauerkraut, to your diet to introduce beneficial bacteria to the gut.
Include prebiotics: Eat foods such as bananas, onions, garlic, and asparagus, which contain prebiotic fibers that nourish the beneficial bacteria in your gut.
Avoid excessive sugar: Limit your intake of high-sugar food and beverges and sugary beverages, as excessive sugar consumption can lead to dysbiosis and related health issues.
Choose natural sugars over non-nutritive sweeteners: If you need to sweeten your food or drinks, opt for natural sweeteners like honey or maple syrup instead of non-nutritive sweeteners.
Stay hydrated: Drinking plenty of water can help keep your gut functioning properly by promoting regular bowel movements and aiding in digestion.
Conclusion: The bitter truth about sugar
High dietary sugar intake can lead to dysbiosis and is linked to various health issues, including obesity, diabetes, and mental health disorders. Maintaining a balanced gut microbiome is essential for overall health, and a diverse, fiber-rich diet, along with prebiotics and probiotics, can support a healthy gastrointestinal environment. By making informed dietary choices and controlling sugar intake, individuals can maintain a healthy gut microbiome and overall well-being.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.