Pseudomonas spp high in stool
Another IBS maker
Over 22% of my IBS cases have revealed elevated P. aeruginosa levels in stool
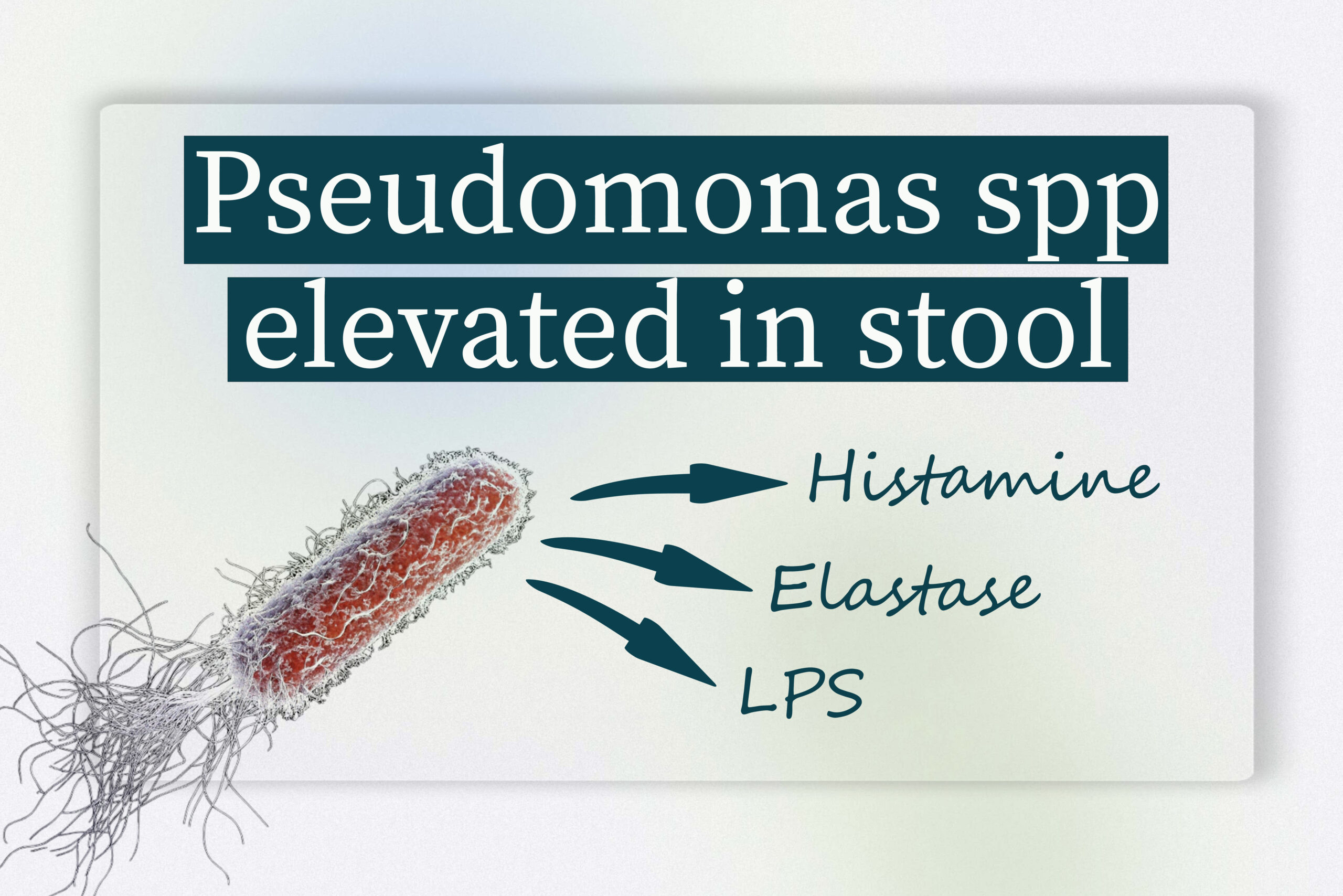
Table of Contents
Pseusomonas spp and most commonly Pseudomonas aeruginosa are a relatively common finding in stool tests of IBS patients. While it is commonly found in soil and water, when it finds favorable conditions, it may thrive and grow within the GI tract. From over 2000 PCR tests assessed in my practice, Pseudomonas spp high in stool has been recovered in about 22% of the cases. And what makes this gram-negative bacterium notorious is the multitude of chemical reactions and enzymatic activities it posseses, from histamine production to gluten degradation.
How often do we find Pseudomonas aeruginosa in IBS patients?
Besides my experience, many studies show that IBS patients display much higher counts of pseudomonas aeruginosa compared to healthy individuals. In duodenal (small intestinal) samples, quantitative PCR analysis showed that IBS patients had an average P. aeruginosa level of 8.3% compared to only 0.1% in healthy subjects—an approximately 83‐fold increase!! Also, in fecal samples, IBS patients exhibited a P. aeruginosa abundance of 2.34% versus only 0.003% in healthy subjects, indicating roughly a 780‐fold higher level!! This is huge.
IBS subtypes
Moreover, when comparing IBS subtypes, in both constipation-predominant (IBS-C) and diarrhea-predominant (IBS-D) patients we find that significantly higher numbers of P. aeruginosa, or antoher Pseudomonas strain, are commonly found in comparison to healthy persons. This suggests that the bacterium’s increased abundance within the gastrointestinal tract is associated with IBS irrespective of the specific symptom pattern.
How does Pseudomonas aeruginosa cause symptoms?

Pseudomonas spp are a kind of bacteria that posseses many activities which may produce symptoms. And all in different levels of gut function; from motility to fermentation. And while other types of bacteria, like Citrobacter spp or Klebsiella spp may colonize predominantly the large intestine, Pseudomonas will thrive easily in the duodenum. Some of the ways this pathogen can interfere with normal gut function are:.
Using serotonin to exploit quorum sensing and antibiotic resistance
Quorum sensing is a very importan function of our gut ecology. It’s essentially the way our gut microbes communicate with each other. High levels of serotonin (which in not always a good thing) in your gut stimulate quorum sensing in Pseudomonas aeruginosa, prompting biofilm formation and the secretion of enzymes that can damage your gut lining. This enhanced bacterial communication may worsen inflammation and complicate an existing infection, making antibiotic strategies more challenging.
Histamine production and chemotaxis
Histamine also plays a role in bacterial signaling. In pseudomonas aeruginosa, histamine modulates gene expression and directs chemotaxis, helping the pathogen get infected by environmental triggers. This process further encourages biofilm development, which is a key factor in sustaining the infection and may even lead to antibiotic resistance.
Antigenic gluten degradation
Usually, gluten is degraded in a manner that most fragments of this protein complex are not harmful. But Pseudomonas possesses a specific elastase activity (in essence, it uses gluten for its own metabolism) and releases fragments that are not recognized by our immune system, thereby promoting constant low-grade inflammation at the site of overgrowth. And since P. aeruginosa colonizes the duodenum (among other sites) it can easily be confused with celiac-like disease. In addition, this is another reason why gluten sensitivity is a real symptom and not in the patients’ minds (as I hear a lot lately).
LPS release in the GI tract
As levels of Pseudomonas aeruginosa rise, it release LPS (Lipopolysaccharide) in the gut lumen which ultimately may enter the bloodstream. When this LPS touches the gut lining—especially in the duodenum—it binds to immune receptors, triggering an inflammatory response. This inflammation makes the gut wall more “leaky” and disrupts normal movement, leading to symptoms that include diarrhea, abdominal pain, bloating, and irregular bowel habits.

find the dedicated chapter oN the treatment of pseudomonas-predominant ibs in ibsyncrasy
Pseudomonas aeruginosa infection and its complications
An untreated pseudomonas aeruginosa overgrowth in your stool can trigger low-grade inflammation and contribute to chronic gastrointestinal discomfort. Clinical observations link high bacteria counts with various IBS symptoms, including abdominal pain and episodes of diarrhea.
Symptom correlation of stool Pseudomonas
When pseudomonas aeruginosa levels are too high, you might experience abdominal pain and occasional diarrhea. My clinical experience has shown that these symptoms often correlate directly with bacterial overgrowth, making it crucial to address the underlying infection before complications— such as a tract infection or even urinary tract infections —arise in individuals whose immune system is weakened.
Post-infectious IBS
Following an acute episode of infection, many patients develop persistent dysbiosis. A pseudomonas aeruginosa overgrowth can set the stage for chronic IBS if the conditions that allowed the bacteria to flourish in the first place are not adequately addressed. Without proper intervention, the bacteria may reappear, highlighting that research is needed into more sustainable treatment strategies.
Actionable steps to manage Pseudomonas overgrowth
So, how do you get rid of pseudomonas aeruginosa in the gut? The answer isn’t simply about taking an antibiotic—it involves a comprehensive strategy that tackles both the infection and the underlying factors that encourage its growth. And while each treatment plan should be highly personalized, some important steps in order to treat pseudomonas aeruginosa are:
Dietary and lifestyle changes against Pseudomonas spp
- Reduce or eliminate gluten: Since pseudomonas elastase may degrade gluten in an antigenic manner, cutting back on gluten can reduce immune triggers.
- Adjust meal timing: As stated earlier, overgrowth of pseudomonas aeruginosa may take place in the small intestine, as well. Avoid eating late at night; late meals may disrupt the migrating motor complex (MMC) in your GI tract and worsen bacterial overgrowth.
- Regular eating schedule: Steer clear of all-day snacking. Continuous calorie intake can feed these bacteria, further aggravating your condition and potentially leading to diarrhea.
- Avoid refined carbs: Refined carbs favor the growth of pseudomonas aeruginosa and also increase the fermentation potential of the dysbiotic environment, producing more gas per gram of carb.
Targeted approaches to reduce Pseudomonas aeruginosa symptoms
- Consider natural antimicrobials: In addition to antibiotics, natural options like oregano oil and berberine can help treat a pseudomonas aeruginosa infection while targeting biofilm formation.
- Biofilm disruptors: These agents work to break down the protective biofilm that the pathogen uses to evade treatment. Breaking this shield can make antibiotics more effective against this pathogen.
It’s essential to address the root causes that allow the infection to persist. Even if you treat the Pseudomonas aeruginosa infection once, if you do not change the conditions that allowed this bacterium to get infected in the first place, overgrowth is likely to recur. Adopting long-term dietary and lifestyle changes is key to keeping these bacteria in check and preventing future episodes.

Theodoros Prevedoros, MSc
The Microbiome Biochemist
With extensive experience evaluating over 3000 cases in various specialties, including gastroenterology, pediatrics, and endocrinology, Theodoros has collaborated with more than 25 doctors from Greece and Cyprus and over 10 laboratories worldwide.
With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.
With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.
More posts