IBS types are not 4... which is yours?
As someone dealing with IBS, you’ve probably experienced a range of frustrations. The emotional distress and impact on your quality of life due to persistent IBS symptoms and the financial burden of ineffective treatments make your situation even more challenging. Feeling isolated, lacking understanding from others (including healthcare professionals), confusion from conflicting dietary and lifestyle advice, and the fear of symptom flare-ups affecting your social and professional life only add to your struggle.
- MISDIAGNOSIS
- MANY DOCTORS - SAME TREATMENT
- DIFFERENT PATIENTS - SAME TREATMENT
- LACK OF UNDERSTANDING FROM DOCTORS AND FRIENDS
- SOCIAL ISOLATION
- CONFLICTING DIETARY AND LIFESTYLE ADVICE
- FINANCIAL BURDEN FOR TESTS AND TREATMENTS

IBSyncrasy
Every IBS is unique
What if there was a revolutionary approach?

IBSyncrasy
Every IBS is unique
An approach that would make you understand what is going on with your gut and give you actionable steps to resolve your IBS once and forever. Introducing the IBSyncrasy classification system: a groundbreaking approach to diagnosing and treating the different types of irritable bowel syndrome (IBS) tailored just for you. Unlike the official nomenclature that classifies IBS based on bowel movement patterns (IBS-D for diarrhea, IBS-C for constipation, IBS-M for mixed, and IBS-U for unclassified), IBSyncrasy takes into account your initial trigger and idiosyncrasy, providing personalized and successful treatments.
By understanding the root cause and considering factors such as specific microbiome changes, hormonal imbalances, enzyme deficiencies, current medical treatments, and environmental culprits, IBSyncrasy offers a new way for you to manage IBS symptoms like abdominal pain, loose stool, constipation, and bloating.
IBS-D, IBS-C, IBS-M: It's just letters for bowel habits

IBSyncrasy
Every IBS is unique
You may already know that the official nomenclature for the four types of IBS is based on bowel movement patterns: IBS-D for diarrhea, IBS-C for constipation, IBS-M for mixed, and an extra IBS-U for unclassified. However, this classification does not provide any information on the cause, mediators, mechanisms, microbiology, or any other useful diagnostic tips. This is why treatments given based on this classification are often average and usually fail.
Limitations of the three types of IBS based on bowel movement patterns

IBSyncrasy
Every IBS is unique
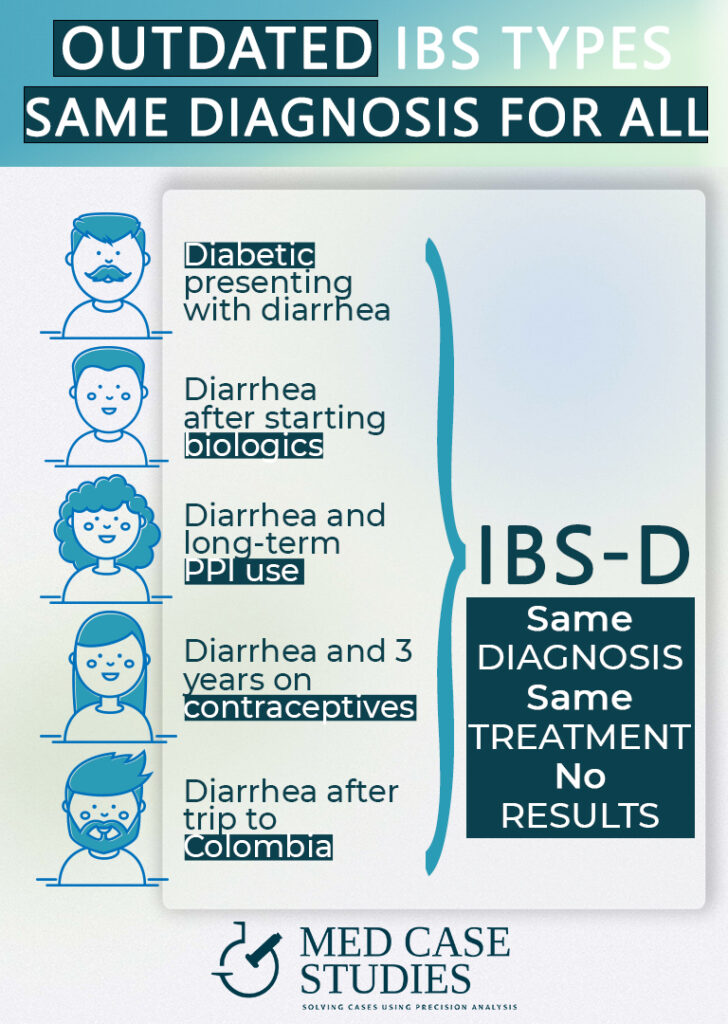
Think of it this way: five different people with IBS go to the gastroenterologist with diarrhea. Each person has their own unique situation, such as being diabetic, taking biologic agents, using PPIs chronically, being a teenager on contraceptives, or having just returned from a trip to Colombia. According to the classic classification system, they would all be diagnosed with IBS-D and given the same treatment, but probably none of them would be cured or at least not for long.
Inadequacy of this system for managing irritable bowel syndrome symptoms

IBSyncrasy
Every IBS is unique
Imagine all the above people going from one healthcare provider to another, only to receive the same treatment for their irritable bowel syndrome (IBS) symptoms, despite the differences in their individual situation. The frustration, emotional distress, and financial burden can be overwhelming. This is precisely the shortcoming of the traditional IBS classification system. The traditional classification system groups IBS symptoms into IBS-C, IBS-D, or IBS-M, but it doesn’t account for the unique factors contributing to everyone’s particular IBS experience.
Regardless if you suffer from post-infectious IBS or small intestinal bacterial overgrowth, you may find yourself receiving the same treatment as others with IBS, even if the underlying cause of your symptoms is entirely different. By not addressing these root causes, the current system leaves you trapped in a cycle of ineffective treatments, adding to the emotional and financial strain of managing your condition.

IBSyncrasy: A paradigm shift in IBS treatment
A Personalized Approach to IBS Management
It’s time for a paradigm shift in IBS treatment, and IBSyncrasy is the answer. By focusing on the initial trigger and the idiosyncrasies of each patient, this groundbreaking classification system offers a wealth of useful diagnostic information to manage and treat IBS. Instead of the traditional one-size-fits-all approach, IBSyncrasy uses extensive clinical data from each individual patient and specific trigger events to provide a personalized IBS type.
IBSyncrasy's Comprehensive Insights
By utilizing the IBSyncrasy classification system, a doctor may gain insights into specific microbiome changes, dysbiosis location (small or large intestine), potential hormonal changes (gastrin, serotonin, etc.), the kind of bacteria involved if there’s mucosal or immune involvement, probable enzyme deficiencies, metabolic imbalances, and hints towards specific environmental culprits. This personalized approach leads to more effective treatments tailored to your unique situation. And it doesn’t matter whether it’s IBS-C or IBS-D, IBS with alternating stool patterns, or any form of IBS.
An example: Management of IBS with diarrhea
- The diabetic patient probably suffers from exocrine pancreatic insufficiency.
- The patient taking biologic agents may have a specific mucosal immunodeficiency.
- The patient taking PPIs chronically most likely has small intestinal bacterial overgrowth (SIBO).
- The teenager’s migrational motor complex may be affected.
- The patient likely has post-infectious IBS, potentially from a tropical parasite.

Targeted Treatments for IBS with Diarrhea
Using these insights, the treatment that is created is highly targeted and addresses the root cause of IBS with diarrhea, rather than simply managing the symptoms. This tailored approach can lead to significant improvements in your digestive health and overall quality of life. IBSyncrasy is a game-changer in the management of IBS, finally offering personalized solutions for those suffering from this complex condition.
Real-world Scenarios: IBSyncrasy in action
A Closer Look at an IBS-D Patient
Let’s dive deeper into the case of a patient taking PPIs for over 3 months and presenting with diarrhea, typically diagnosed as IBS-D. Under the classic classification system, this patient would be prescribed rifaximin, a common anti-diarrhea treatment, and possibly a probiotic. However, this treatment fails to recognize most of the underlying issues, such as small intestinal bacterial overgrowth (SIBO), constant gastrin elevation, chronic gastric acid suppression due to PPI administration, and long-term histamine release from the stomach to counterbalance the acid suppression. Ignoring these diagnostic clues from the patient’s IBSyncrasy can lead to temporary relief, while symptoms may relapse, potentially even worse than before.
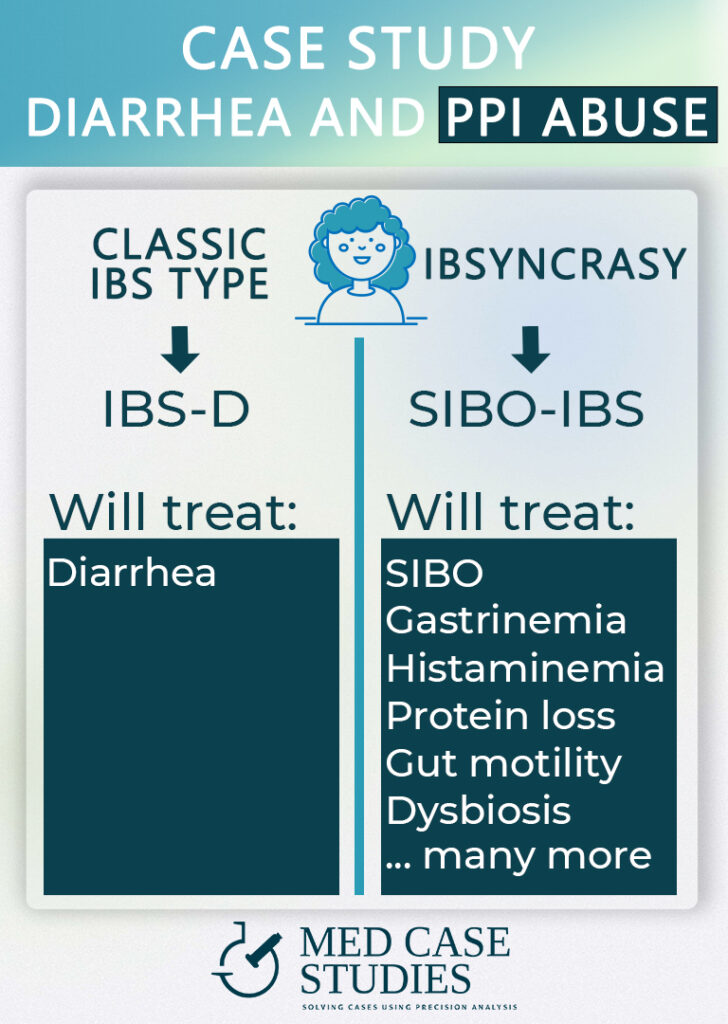
IBSyncrasy's Treatment Approach
Using the IBSyncrasy system may develop a more comprehensive treatment plan for each patient. In addition to rifaximin, the patient’s stomach medicine may be changed or stopped, probiotics will be avoided for at least 3 months, and a specific diet to reduce SIBO (low-FODMAP and low-gluten due to duodenal villi being part of the problem) will be recommended. The patient will also be given mucosal nutrients and a list of five behavioral interventions to help achieve a long-term cure.
Long-term Symptom Relief with IBSyncrasy
This personalized approach creates the conditions for the patient to not only feel better in the short term but to maintain their improved health and relief from the symptoms of IBS in the long-term. By addressing the root causes and unique factors that contribute to their IBS, the patient can experience lasting relief from gastrointestinal symptoms, such as abdominal pain, bloating, and changes in stool consistency. This innovative approach takes into account all the specific aspects of your digestive tract, and not just the impact of certain foods on your symptoms, and offers a more holistic and effective treatment plan. By addressing the underlying causes of your IBS, you can experience significant improvements in your symptoms and overall quality of life.
IBSyncrasies: New and different types of IBS
Experience with IBS: 2100 Cases and Counting
With extensive experience handling over 2100 cases of irritable bowel syndrome (IBS), I have been able to identify at least 28 unique IBSyncrasies. This comprehensive understanding of the various subtypes of IBS allows for a more personalized and effective approach to treatment, as opposed to the classic classification system based on bowel movement patterns.
10 Common IBSyncrasies and Their Characteristics
The 10 most common IBSyncrasies, each with a specific characteristic that might be missed using the classic classification system, include:
- Post Infectious IBS – Enhanced visceral hypersensitivity: This subtype of IBS occurs after a gastrointestinal infection and often presents with heightened sensitivity to pain and discomfort in the digestive tract.
- Postcholecystectomy syndrome – Altered mucosal pH: Following gallbladder removal, some patients experience IBS symptoms due to changes in the pH levels in the gastrointestinal tract. This can lead to either constipation or diarrhea.
- Prostatitis IBS – Antibiotics for prostatitis: In men, chronic prostatitis can be associated with IBS, leading to a mix of constipation and diarrhea and sometimes loose stool
- Pseudomonas IBS – Gluten elastase activity: This IBS subtype is characterized by the presence of Pseudomonas bacteria, which produce elastase that can break down gluten, leading to diarrhea and stomach pain.
- PPI IBS – Hypergastrinemia-SIBO: Long-term use of proton pump inhibitors (PPIs) can cause elevated gastrin levels, SIBO and malabsorption.
- Proteus IBS – Microbes thriving on glutamine (diarrhea): The presence of Proteus bacteria in the intestine can lead to diarrhea due to their preference for glutamine, an amino acid that makes them swarm. This type of IBS may be one of the hardest to diagnose.
- Pediatric IBS – Immature GI development (ibs with mixed bowel): In children, an underdeveloped digestive system can lead to IBS symptoms, often with a mix of constipation and diarrhea.
- SIBO IBS – Different enzyme activities (constipation or diarrhea): Small intestinal bacterial overgrowth (SIBO) can cause IBS symptoms by altering the activity of digestive enzymes, resulting in either constipation or diarrhea and several times lumpy stool.
- Exocrine pancreatic insufficiency IBS – Enzyme adequacy (ibs with constipation): Insufficient production of digestive enzymes by the pancreas can lead to IBS with constipation. This may be identified by simple stool tests
- Immunodeficiency IBS – Inadequate mucosal immunity, dysbiosis (diarrhea and constipation): A weakened immune system can result in an imbalanced gut microbiome, contributing to both diarrhea and constipation in IBS sufferers.
Understanding these different IBSyncrasies allows for tailored treatment plans that address the root causes and unique factors contributing to each patient’s IBS symptoms, ultimately improving the management and quality of life for those living with this complex condition.
FAQ
Are there different types of IBS?
Yes, there are different types of IBS, characterized by various symptoms associated with abnormal bowel movements. They can be categorized based on bowel movement patterns, such as constipation and diarrhea (IBS-C and IBS-D, respectively) and mixed (IBS-M). Additionally, IBS subtypes can be identified based on the initial trigger, such as post-infectious IBS (PI-IBS), PPI-IBS, Proteus-predominant IBS, and post-cholecystectomy IBS (following gallbladder removal). Recognizing the specific subtype can help tailor strategies to help relieve symptoms of abnormal bowel patterns
Can IBS be mistaken for something else?
IBS can be mistaken for other conditions due to its varying presentation, influenced by factors such as the initial trigger, patient’s microbiome before onset, dietary habits, and current medicines. The development of IBS is unique to each individual, leading to diverse GI symptoms that can mimic other disorders. While there is no single cure for IBS, understanding these contributing factors can help in tailoring appropriate treatment and management strategies.
Can IBS change types?
Absolutely! IBS can indeed change types as it evolves with shifting symptom patterns. These changes in your bowel movements may be influenced by microbiome changes and hormonal inputs. It’s not uncommon for individuals to experience varying degrees of similar symptoms such as gas and bloating or changes in bowel movements over time.
Is stress making my IBS worse?
While stress isn’t typically the root cause, it can certainly aggravate the IBS you’re dealing with. When stressed, you may experience intensified symptoms, as stress hormones can exacerbate processes within the gut. In fact, many people with IBS notice a connection between stress and an IBS flare-up. The main factors influenced by stress include the microbiome, the enteric nervous system, and the visceral sensitivity system, among other hormonal inputs. Being mindful of stress levels can help alleviate pain and distress associated with IBS symptoms.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.