Hypothyroidism and SIBO
The link betwwen thyroid heatlh and small intestinal bacterial overgrowth
💬 Have a question? Use the live chat in the bottom-right to ask me anything in real time.
Hypothyroidism and SIBO coexist in over 54% of my cases of severe small intestinal bacterial overgrowth
Table of Contents
You might have noticed that whenever your thyroid starts to act up, your gut throws a tantrum too. Trust me, you’re not overreacting. As a functional medicine practitioner and microbiome researcher who has worked with over 4,000 cases, I’ve seen this pattern far too often to call it coincidence. Even slight shifts in thyroid hormone levels can create a ripple effect through your digestive system. The gut and the thyroid are in constant biochemical dialogue. Just like in classic irritable bowel syndrome, when one gets off script, the other tends to spiral.
In hypothyroidism, the fragile balance inside your small intestine often breaks down. This is when Small Intestinal Bacterial Overgrowth (SIBO) shows up—a condition where bacteria in your small intestine multiply in places they’re not meant to. The overgrowth of bacteria becomes a direct trigger for bloating, food sensitivities, and unpredictable diarrhea or constipation. I’ve witnessed time and again how SIBO becomes the missing piece in people with thyroid disease who can’t seem to stabilize, no matter how clean they eat or how carefully they dose their thyroid medication.
SIBO is not rare in people with a thyroid condition. It’s actually pretty common. And yet, most treatment plans don’t address it at all.
The Gut-Thyroid connection: Symptoms of SIBO
Now that the pattern is clear, let’s see how your thyroid and gut interact so closely. When thyroid hormone levels drop—especially FT4—you’ll often see corresponding spikes in hydrogen and methane on a breath test. These gases reflect bacterial overgrowth and altered metabolism inside your small intestine. That’s why testing for SIBO is so valuable, especially if your gut is struggling and your thyroid levels are fluctuating.
In early pregnancy, 57% of women with subclinical hypothyroidism test positive for SIBO. That’s not just a small overlap. It’s a biochemical collision. If you’ve dealt with IBS-like symptoms—bloating, pain, diarrhea, irregular stools—but you also have hypothyroidism, the two are probably connected. Based on thousands of breath tests I’ve reviewed, about 54% of people with overt hypothyroidism have SIBO.
Let me put it simply: SIBO often coexists with abnormal thyroid levels. You don’t have two separate issues. You have one miscommunication happening across two systems. And if your doctor isn’t connecting the dots, you’re going to keep running in circles.
Mechanisms linking hypothyroidism and small intestinal bacterial overgrowth
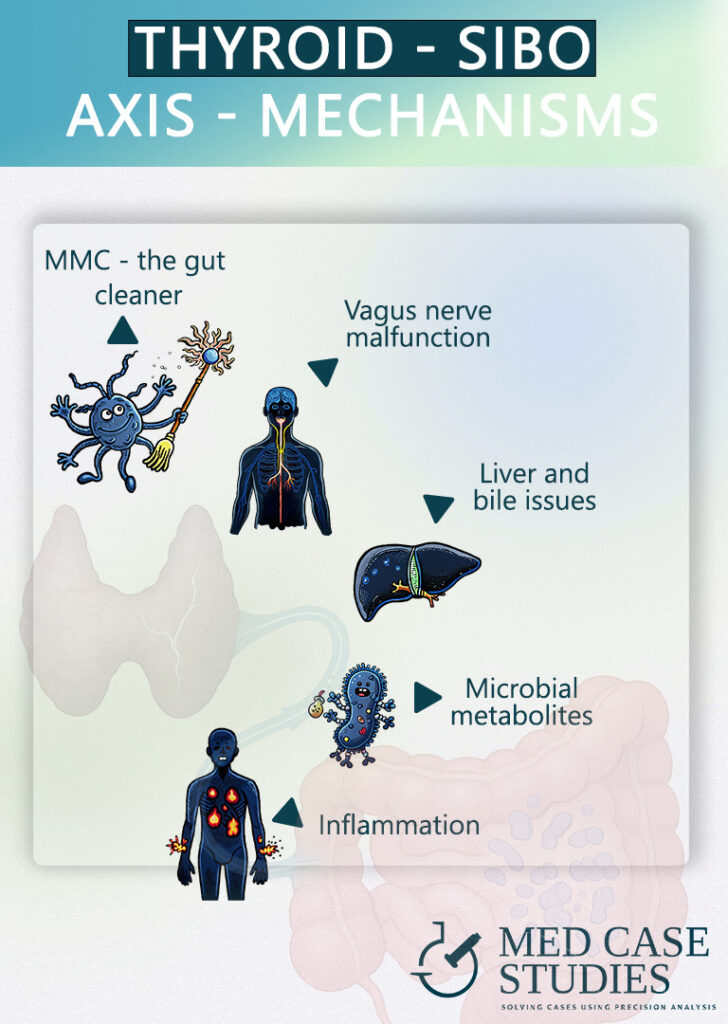
Let’s look under the hood and see what’s actually causing this gut-thyroid chaos. The relationship between hypothyroidism and small intestinal bacterial overgrowth isn’t theoretical—it’s mechanical, neural, and biochemical. So, to make it simple, I divide the mechanisms into three buckets: motility regulation, neurohormonal signaling, and biochemical feedback loops.
Motility Regulation: The MMC and Bacterial Clearance
Gut health relies heavily in a process called the Migrating Motor Complex (MMC), which essentially is your gut’s housekeeping team. When it’s working, it quietly sweeps debris and excess bacteria down your digestive tract between meals. But it only activates if you leave enough time between meals. If you’re grazing or snacking constantly, you’re shutting down the MMC. And if the MMC gets shut down too often, bacteria in the gut take the opportunity to settle where they don’t belong—hello SIBO.
I’ve seen countless patients unknowingly sabotage their gut’s natural cleaning cycles. Add in gallbladder removal or long-term use of proton pump inhibitors (PPIs), and now you’ve got a serious motility problem. Many of these patients eventually develop SIBO, and almost always, there’s some degree of hypothyroidism in the background.
Neural and thyroid health: The role of the vagus nerve and motilin
Next, we’ve got the vagus nerve—your gut-brain communication line. When vagal tone drops due to chronic stress, medications like atropine, or poor sleep, gut motility suffers. The signals stop firing, and your MMC stays stuck in neutral.
Then there’s motilin, a hormone secreted in the duodenum that jumpstarts those critical phase III MMC contractions. If you’ve had your gallbladder removed, your motilin levels likely dropped. That affects how quickly your gut moves and whether bacteria in your small intestine stick around longer than they should.
Biochemical disturbances: Bile acids, inflammation, and microbial metabolites
Each digestive cycle releases bile acids. They help you digest fats, but they’re also caustic and can damage intestinal lining if they linger. That damage normally triggers tissue repair—but without a functioning MMC, that repair never happens. Instead, you get low-grade inflammation that helps SIBO flourish.
What’s more, microbial byproducts—like LPS—released by bacteria in the small intestine can interfere with thyroid hormone conversion and receptor sensitivity. It creates a vicious feedback loop: hypothyroidism may impair motility and digestion, which causes SIBO; and SIBO, in turn, interferes with how your body uses thyroid metabolites.
This is where I often find the true root cause of persistent symptoms hiding—not in the lab results, but in the interactions between your gut bugs and your hormones.
SIBO and your thyroid: The interdependent balance
If your thyroid function is off, your gut slows down. When your gut slows down, SIBO shows up. And once SIBO is present, it inflames the lining of your gut and interferes with the absorption of your thyroid medication. So even if you’re taking the right dose, it may not be doing its job.
Here’s the kicker: SIBO can also trigger immune responses that disrupt hormone signaling across your entire endocrine system. Bacterial byproducts like LPS act like little inflammatory messengers, getting into your bloodstream and jamming up your hormonal gears.
I’ve seen so many people try to fix just their gut, or only their thyroid, and wonder why they’re still bloated, exhausted, or foggy. Real healing only happens when you address both ends of the axis. You can’t fix the plumbing if the water supply is broken—and vice versa.
SIBO and hypothyroidism case study: Colin's case
Colin’s real-life clinical story, chosen from many similar cases in my practice, illustrates precisely why treating your thyroid and gut together is essential.
Colin came in feeling like he’d tried everything. He was on long-term thyroid medication, eating what he thought was a clean diet, and yet his bloating, fatigue, and IBS-like symptoms just wouldn’t quit.
His lab results were unpredictable. His digestion was sluggish. Some days were okay, but most were just frustrating. He began to wonder if it was all in his head.
We ran a SIBO test and found a classic overgrowth pattern—gas production aligned perfectly with his symptoms. But treating the SIBO with antibiotics alone wasn’t enough. We had to work on meal spacing, vagal nerve stimulation, dietary consistency, and a few key stress management practices to regulate the gut–thyroid axis.
Once we addressed both the SIBO and the thyroid condition—not just one or the other—everything started to improve. His thyroid hormone levels stabilized. His symptoms of SIBO, including bloating and intermittent diarrhea, decreased dramatically. And most importantly, he felt like himself again. Not overnight, but steadily and sustainably.
Colin’s case isn’t rare. I’ve worked with hundreds like him. What makes the difference is treating both systems together—because they never stopped working together in the first place.
SIBO treatment options
Now you might be thinking, “Okay, I see the connection. What now?” Here’s what I recommend—step by step—after seeing thousands of patients with hypothyroidism and small intestinal bacterial issues.
Probiotics: But won’t they worsen SIBO?
This question comes up constantly. People are understandably nervous: “Won’t probiotics feed the bacteria in the small intestine and make SIBO worse?” The answer, surprisingly, is no—if you use the right strains.
According to a large meta-analysis, probiotics alone resolved SIBO in 53% of cases. And when paired with antibiotics, the success rate jumped to 86%. So, treating SIBO with probiotics isn’t just safe—it’s often more effective than using antibiotics alone. In fact, probiotics help reduce gas production, inflammation, and the severity of symptoms of SIBO.
The best results I’ve seen involve blends containing Bifidobacterium infantis, Lactobacillus acidophilus, Enterococcus faecalis, and Bacillus cereus. These strains calm immune reactivity, strengthen the gut barrier, and help with overall gut health—all without promoting bacterial overgrowth in the wrong place.
Timing matters: No more late-night meals
Your gut has a schedule. And when you eat too late, you throw it completely off. Every meal you eat triggers insulin and suppresses motilin—the hormone that activates your MMC. So if you’re snacking late or eating dinner at 10 p.m., your gut’s natural cleaning cycles don’t have a chance to run.
That’s why one of my go-to first steps is extending the overnight fast to at least 12 hours. No food after 8 p.m. If you’re eating dinner at 9 or 10, that’s a problem. Your motility suffers, and SIBO flares up. I’ve seen this change alone dramatically improve bloating and reduce gas production in patients struggling with hypothyroidism.
Medicated treatment of SIBO
Here’s something that doesn’t get talked about enough: SIBO can also reduce the absorption of your thyroid medication. If you’ve been on levothyroxine and your dose keeps creeping up, that may not be because your thyroid is getting worse—it could be that inflammation and microbial overgrowth in your small intestine are preventing proper absorption.
In many cases, especially when symptoms are severe, I’ll use rifaximin—a targeted antibiotic that works specifically in the small intestine. It helps knock down the bacterial overgrowth and creates a window of opportunity for medication absorption to rebound. But here’s the key: antibiotics alone won’t keep SIBO from coming back. You have to change the environment that allowed it to grow in the first place.
That’s where everything else—MMC restoration, meal timing, stress support, and probiotics—comes into play. They’re not optional. They’re essential to long-term success.
Consistent dietary patterns – Beyond FODMAPs Diet
Let’s talk food. Yes, diet matters—but no, it’s not all about restriction. While many patients with SIBO do temporarily benefit from a FODMAPs diet, I’ve found that consistency is far more important than perfection.
Radical diet shifts every few weeks can confuse your microbiome and derail your progress. Your gut bugs thrive on routine. That’s why I recommend sticking to a rhythm—not just in what you eat, but when you eat it. This keeps your MMC working, supports stable blood sugar, and encourages balanced gut bacteria.
But food isn’t the only factor. Your nervous system, sleep patterns, and emotional stress also impact both your gut and your thyroid health. That’s why I always bring lifestyle into the picture. Structured meal timing, restorative sleep, and simple tools like diaphragmatic breathing or vagal tone exercises can make the difference between relapse and recovery.
As shown in Colin’s story, it’s the combination of medical strategy and lifestyle integration that creates lasting results—not just a temporary fix.
FAQ: Hypothyroidism and SIBO
How are hypothyroidism and SIBO connected?
Hypothyroidism slows gut motility (the MMC), which lets bacteria linger and overgrow in the small intestine (SIBO). The relationship is two-way: SIBO’s byproducts can also interfere with thyroid hormone metabolism. On this page you note that ~54% of people with overt hypothyroidism have SIBO, and that 57% with subclinical hypothyroidism in early pregnancy test positive for SIBO.
Does SIBO affect thyroid medication absorption?
Yes. Once SIBO is present it inflames the gut lining and can interfere with levothyroxine absorption, so even a correct dose may not work as expected. Treating SIBO helps medication absorb and perform better.
Won’t probiotics make SIBO worse?
No, when used correctly. You cite a large meta-analysis where probiotics alone resolved SIBO in ~53% of cases and ~86% when combined with antibiotics. Targeted blends can reduce gas, inflammation, and symptoms without worsening overgrowth.
What habits help restore gut motility (MMC)?
Allow time between meals, avoid late-night eating, and aim for a ~12-hour overnight fast. Support vagal tone, sleep, and stress management. Gallbladder removal or long-term PPIs can impair motility and raise SIBO risk.So meal timing and lifestyle are essential.
How do you treat SIBO when you also have hypothyroidism?
Treat both together. Depending on severity, use a targeted antibiotic like rifaximin, plus a probiotic regimen, structured meal spacing, vagal tone work, and consistent diet patterns. Optimizing thyroid medication alongside gut treatment improves outcomes and reduces relapse.
Conclusion
Colin’s case might sound a lot like yours. And it’s not unique. I’ve worked with hundreds of people who’ve spent years treating symptoms—of IBS, hypothyroidism, anxiety, or bloating—without ever realizing that their thyroid and gut were locked in a dysfunctional loop.
SIBO isn’t just a nuisance. Left untreated, it can block thyroid hormone absorption, mimic or worsen IBS, elevate systemic inflammation, and lead to unnecessary increases in medication dosages. On the flip side, hypothyroidism can directly cause the slow motility that allows SIBO to develop.
This isn’t just theory. This is what I’ve seen, again and again, in real people with real symptoms.
The solution? Treat both the gut and the thyroid at the same time. Address the root cause, not just the result. Support motility. Rebuild the MMC. Fix vagal tone. Adjust food timing. Use evidence-based probiotics. And when necessary, use pharmaceuticals like rifaximin with a long-term recovery plan in place.
SIBO may be stubborn, but it’s not unbeatable. Especially when you understand the full picture—and treat the gut-thyroid axis like the dynamic, reciprocal system that it is.

Theodoros Prevedoros, MSc
The Microbiome Biochemist
With extensive experience evaluating over 3000 cases in various specialties, including gastroenterology, pediatrics, and endocrinology, Theodoros has collaborated with more than 25 doctors from Greece and Cyprus and over 10 laboratories worldwide.
With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.
With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.
More posts


