
GABA is a valuable part of the treatment in 2 of the ibsyncrasies detailed and resolved in the book

IBSyncrasy
Every IBS is unique
With a global estimated prevalence rate of 10-20%, Irritable Bowel Syndrome (IBS) is a widespread gastrointestinal disorder that can profoundly affect the quality of life. IBS has historically been a challenging condition to comprehend due to its multifaceted origins. However, recent studies have made significant strides toward demystifying this ailment. A crucial factor that has emerged is our gut microbiota, the residents of the gastrointestinal tract.

IBSyncrasy
Every IBS is unique
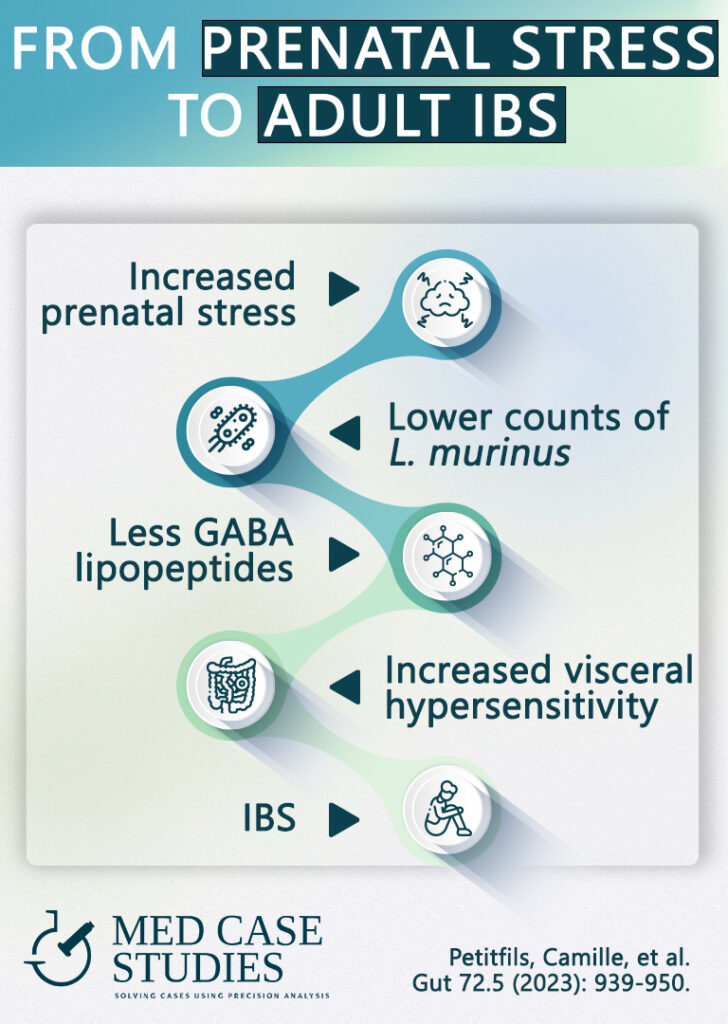
The study leveraged a mouse model to investigate the role of prenatal stress (PS) on gut microbiota and visceral hypersensitivity. Visceral hypersensitivity, or an amplified pain response to stimuli in the gut, is a typical symptom in IBS patients. The team then employed mass spectrometry to quantify the production of GABA-containing lipopeptides in a particular strain of gut bacteria, the mice’s colons, and in fecal samples from human IBS patients and healthy volunteers.

IBSyncrasy
Every IBS is unique
In mice exposed to renatal stress (PS), researchers observed dysbiosis characterized by a decrease in the abundance of a specific bacterial species called Ligilactobacillus murinus. This bacterial shift inversely correlated with visceral hypersensitivity; as the bacteria’s population dwindled, the mice’s pain response increased.
What’s even more fascinating is that the Ligilactobacillus murinus produced lipopeptides containing GABA, including one named C14AsnGABA. When the researchers treated PS-induced mice with this lipopeptide, it resulted in a reduction in visceral sensitivity to colorectal distension (CRD), a measure of visceral pain!

IBSyncrasy
Every IBS is unique
In human samples, researchers found a similar pattern. The concentration of C16LeuGABA, another GABA-containing lipopeptide, was notably lower in IBS patients compared to healthy individuals. Notably, this lipopeptide demonstrated an inhibitory effect on sensory neuron activation, potentially explaining its role in reducing visceral pain.
While this study provides persuasive evidence, it’s critical to remember that IBS is a complex disorder with multiple contributing factors. Other research has pointed towards different bacterial strains, diet, and even genetics as potential influencers. For instance, some studies have found an overgrowth of certain bacteria, such as Escherichia coli, in IBS patients. Therefore, understanding and treating IBS likely involves addressing an array of elements.

Eating behaviors and the gut microbiome
Given the role of gut bacteria in IBS, dietary changes that promote a healthy microbiome could prove beneficial. Including prebiotic and probiotic foods, like yogurt, kefir, and fermented vegetables, may help support beneficial gut bacteria. In addition, several eating behaviors and everyday habits influence the development and optimization of the gut microbiome. Reducing stress is a common phrase but not easy to implement. In the following sections, some very specific tips to increase GABA will be described.
This groundbreaking study highlights the potential of bacterial lipopeptides, specifically those containing GABA, in modulating visceral hypersensitivity in IBS. It also emphasizes the subtle yet crucial role that early-life stress might play in predisposing individuals to the condition.

Post Infectious IBS
Success case study
Based on my experience, GABA indeed proves to be a useful adjunctive treatment for those grappling with irritable bowel syndrome whose symptoms are exacerbated by stress. GABA, or gamma-aminobutyric acid, is a vital molecule that regulates the vagus nerve and almost the entire enteric nervous system. Especially in cases where IBS is triggered by an infection, it is very helpful in reestablishing a normal gut-brain axis. It plays a significant role in managing intestinal motility, an essential component when addressing IBS.
When the functioning of the intestinal tract becomes irregular, it can cause IBS and trigger a variety of symptoms. These can range from altered bowel movements to constipation, making life uncomfortable for many individuals. GABA’s influence on the nervous system can help alleviate these problems.
One of the primary ways GABA aids those with IBS is by helping to regulate abdominal discomfort and the frequency of bowel movements. By reducing the irregularity, it can also help alleviate constipation, a common symptom of IBS. Additionally, GABA’s role in the regulation of intestinal motility helps to manage stool consistency and frequency. This function is crucial in providing relief from the uncomfortable feeling of bloat that often accompanies IBS.
IBSyncrasy
Find your IBS type
Mindfulness meditation is one way to manage stress and boost GABA levels, helping to calm an overactive gut and reduce the discomfort associated with all IBS types. When GABA levels are low (a situation that can occur due to major life events or stress), it can lead to the development of IBS. Lower GABA levels can make our gut overly active, leading to symptoms of IBS like irregular bowel movements and abdominal pain.
Regular resistance exercise is a helpful approach for people with IBS. Resistance exercise aids the central nervous system in boosting the production of a helpful substance called BDNF, which in turn increases GABA levels helping both stress and IBS. This increase in GABA can restore balance in the gut, reducing inflammation and easing the discomfort associated with any gastrointestinal disease.
Deep breathing exercises can counteract the motility issues that GABA deficiency may cause. GABA deficiency leads to an overactive response in cells known as mast cells, a situation that is known to contribute to IBS. When these cells become overactive, they release substances like histamines that lead to inflammation and discomfort in the gut. This response can worsen IBS symptoms and other functional bowel disorders associated with anxiety and depression.
Low levels of GABA can cause an overproduction of serotonin by certain cells in the gut, a situation that can trigger IBS by leading to common gut symptoms like increased bowel motility and discomfort. This scenario is an example of how life stress disrupts intestinal homeostasis by creating hormonal imbalances that contribute to developing IBS. Drinking peppermint herbal tea can help alleviate these symptoms. The tea contains menthol, a substance that can reduce overactivity in the gut, thereby easing the discomfort associated with IBS. This illustrates how simple interventions can help manage the condition, even though IBS may initially appear challenging to tackle.
Yes, stress during early life can contribute to the development of irritable bowel syndrome. The impact of early life adversity, such as stress, can disrupt gut homeostasis and alter the balance of gut microbiota. This alteration has been linked in patients with irritable bowel syndrome. The study highlights the link of childhood stress to the development of IBS, underlining the importance of early life experiences in shaping our gut health.

| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |