What triggers IBS flare ups?
What is an IBS flare-up or attack and its mechanisms?

IBSyncrasy
Every IBS is unique
Flare-ups, those times when your symptoms get a real attitude, can feel like your body’s version of a tantrum, turning ordinary tasks into daunting challenges. While the mechanisms of IBS flare-ups are limited, the triggers that may set them off are too many. And recognizing these triggers is key to managing them in the long term. But first, let’s take a brief look at the main IBS flare-up mechanisms. The precise mechanisms leading to an IBS flare-up are intricate, involving a combination of factors related to visceral hypersensitivity, gut spasticity, and gut secretory dysfunction.
The underlying mechanisms of IBS flare-ups

IBSyncrasy
Every IBS is unique
Visceral hypersensitivity refers to an increased sensitivity to stimuli in the gut. For instance, distension in the gut due to gas or stool might cause discomfort or pain in someone with IBS, while a person without IBS wouldn’t perceive this as painful. This hypersensitivity is thought to involve changes in pain-signaling pathways within the nervous system, such as increased expression of the nerve growth factor gene, which can lead to increased sensitivity to pain in the gut.
Gut spasticity alludes to abnormal contractions in the smooth muscle of the digestive tract, disrupting the rhythmic movement of the gut (peristalsis) needed for normal digestion and the passage of stool. This could be influenced by alterations in certain muscle contractility-related proteins like myosin and actin within the smooth muscle cells.
Gut secretory dysfunction implies an imbalance in the secretion of fluids and electrolytes in the gut. This is often tied to changes in chloride ion secretion mediated by the CFTR ion channel and electrolyte absorption mediated by the NHE3 protein, leading to either constipation or diarrhea.
What are the most common IBS symptoms?
The unpredictable terrain of IBS symptoms during a flare

Milk composition updates daily
When you’re living with IBS, every day can feel like a guessing game. From unexpected bouts of abdominal pain to embarrassing gas issues, it can seem like your gut has its own mind. The most common symptoms of IBS include sudden changes in bowel movement, where one might experience constipation (IBS-C), diarrhea (IBS-D), or both (IBS-M). Feeling bloated or having painful cramps are also common experiences, and to top it off, you might encounter a mysterious symptom – your food seems to cause gas more often than before!
Causes of Irritable Bowel Syndrome flare-ups

IBSyncrasy
Every IBS is unique
The main trigger-causes of IBS may be divided into 4 major categories. 5 culprits from each category are presented in the following section.
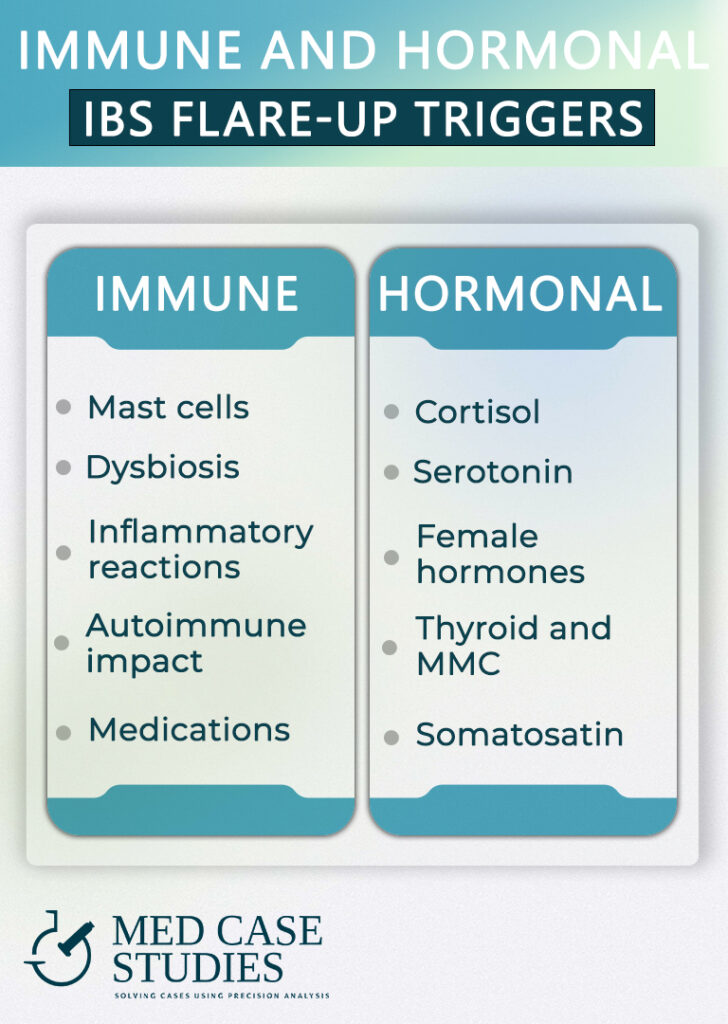
Immune related triggers
- Mast cells
- Dysbiosis
- Inflammatory reactions
- Autoimmune impact
- Medication induced
MAST CELL ACTIVATION

IBSyncrasy
Every IBS is unique
As someone experiencing IBS, you might wonder what your seasonal allergies have to do with your gut troubles. Interestingly, mast cells play a crucial role in both. When aggravated by allergies, these immune cells undergo a process called degranulation, leading to increased histamine release. As a potent compound involved in allergic reactions, histamine can incite an upheaval of your IBS, making symptoms come and go with varying intensity.
DYSBIOSIS

IBSyncrasy
Every IBS is unique
The balance in your gut microbiota can tip following a course of antibiotics, leading to bacterial overgrowth, a phenomenon that holds the potential to accentuate IBS discomfort. Biochemically, these bacteria can produce various metabolic byproducts like gas, endotoxins, and short-chain fatty acids that can irritate the gut lining and cause gas, cramping, and alternations in bowel movements, adding to the complexities people with IBS endure.
INFLAMMATORY REACTIONS

IBSyncrasy
Every IBS is unique
Chronic stress can subtly yet significantly impact your gut health. It can incite your immune system to overreact, triggering an inflammatory response in the intestines. This inflammation can cause your gut to become hypersensitive and hyperreactive to normal stimuli, making the symptoms of IBS vary from person to person and becoming particularly distressing during stress-inducing situations.
AUTOIMMUNE IMPACT

IBSyncrasy
Every IBS is unique
For those dealing with autoimmune disorders, the plot thickens. Such conditions can lead to immune-mediated damage to the enteric nervous system – your gut’s very own nervous system. This can disrupt the normal communication between your gut and brain, exacerbating the intensity and frequency of IBS upheavals.
MEDICATION INDUCED

IBSyncrasy
Every IBS is unique
Lastly, it might surprise you to learn that regular consumption of non-steroidal anti-inflammatory drugs (NSAIDs) can make IBS more challenging. These commonly used pain relievers can lead to increased intestinal permeability, often referred to as “leaky gut,” allowing substances that should stay inside the gut to escape into the bloodstream, triggering an immune response and making IBS more difficult to manage.
Hormone related triggers
- Cortisol and stress
- Estrogen, progesterone and the “cycle”-IBS
- Serotonin imbalances
- Thyroid and MMC
- Somatostatin and aging
CORTISOL AND STRESS

IBSyncrasy
Every IBS is unique
From a gastroenterology perspective, the role of hormones in IBS is striking. Let’s start with cortisol, a hormone primarily known for managing our body’s response to stress. Over time, chronic stress can lead to an overproduction of cortisol, which can disrupt gut motility. This disruption particularly affects the small intestine, where most digestion occurs. Changes in gut motility could cause bouts of IBS, making symptoms such as pain and discomfort worse and possibly diminishing one’s quality of life.
FEMALE HORMONES

IBSyncrasy
Every IBS is unique
Women might notice a fluctuation in their IBS conditions during their menstrual cycle. This is largely due to the hormonal interplay of estrogen and progesterone, which can influence gut motility. Specifically, high levels of these hormones may lead to slower gut transit, causing constipation, whereas low levels can speed up transit, leading to diarrhea. Understanding these fluctuations can play a crucial role in the personalized management of IBS.
SEROTONIN IMBALANCES

IBSyncrasy
Every IBS is unique
Serotonin, often dubbed the “happiness hormone,” also plays a key role in the regulation of bowel movements. Lack of sunlight exposure, particularly during the shorter days of winter, can lead to decreased serotonin production, potentially leading to IBS exacerbations. Interestingly, about 90% of serotonin is produced in the gut, further emphasizing its connection to IBS.
THYROID AND MMC

IBSyncrasy
Every IBS is unique
Disrupted thyroid function may impact the Migrating Motor Complex (MMC), the cyclic pattern of electrical activity in the digestive tract, resulting in irregular gut motility. This irregularity can lead to disturbances in intestinal transit times, fostering conditions like bacterial overgrowth or dysbiosis, which can stimulate IBS flare-ups. Additionally, thyroid hormone fluctuations can alter the gut-brain axis, possibly exacerbating stress-related IBS flare-ups.
SOMATOSTATIN AND AGING

IBSyncrasy
Every IBS is unique
Finally, with aging comes increased production of somatostatin, a hormone known to slow down gut motility. In excess, it can cause food to stay in the intestines longer than usual, potentially causing discomfort and making IBS harder to manage.

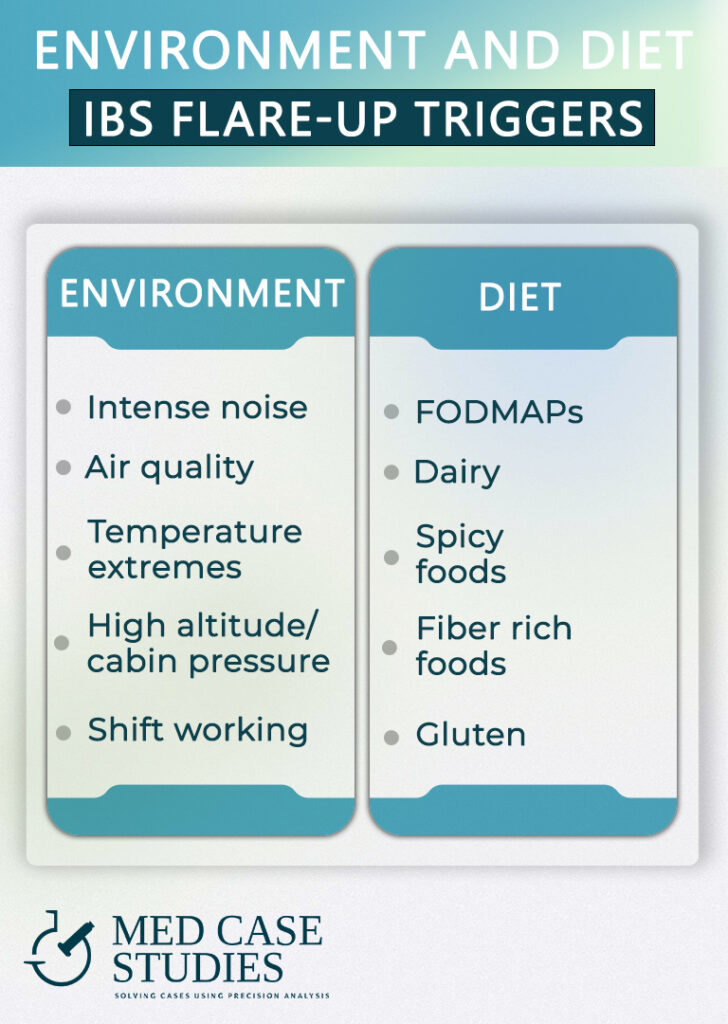
Diet related triggers
- FODMAPs
- Dairy
- Gluten
- Fiber
- Spicy foods
FODMAPs

IBSyncrasy
Every IBS is unique
First on our list are FODMAPs – Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are types of carbohydrates found in a wide variety of foods. High FODMAP foods, such as certain fruits and vegetables (for instance, a peach), can create an osmotic effect and fermentation in the gut. This process leads to distension which can instigate an uncomfortable IBS event.
DAIRY

IBSyncrasy
Every IBS is unique
In addition to FODMAPs, dairy products, especially those high in lactose, can worsen IBS in lactose-intolerant or disaccharidase deficient individuals. When lactose is not properly digested, it ends up in the colon where it ferments, producing gas and leading to symptoms such as bloating and diarrhea.
GLUTEN

IBSyncrasy
Every IBS is unique
Gluten is another dietary component that can influence IBS. In people with non-celiac gluten sensitivity, gluten consumption can stimulate an immune response and inflammation in the gut, potentially setting off an IBS episode. In addition, colonization of the small intestine with Pseudomonas aeruginosa, makes gluten antigenic in the absence of gluten intolerance.
FIBER

IBSyncrasy
Every IBS is unique
Fiber intake also plays a critical role in IBS. A diet low in fiber can slow gut transit times, leading to constipation. Consuming sufficient fiber, particularly from fruits and vegetables, is key to maintaining regular bowel movements. On the other hand, excessive consumption of raw fiber may induce an IBS flare-up, mainly bloating. Balance is key when it comes to fiber.
SPICY FOODS

IBSyncrasy
Every IBS is unique
Lastly, the consumption of spicy foods, which can be considered trigger foods, may irritate the gut lining, causing diarrhea and cramping in some IBS patients. Consumption of spicy foods is directly associated with IBS, particularly in women.
Environment related triggers
- Noise pollution
- Air quality
- Shift working
- Temperature extremes
- High altitude and cabin pressure
NOISE POLLUTION

IBSyncrasy
Every IBS is unique
The unseen, yet ever-present, environmental factors that can trigger IBS. You might not consider noise pollution as a potential agitator of your gut, but exposure to high levels of noise pollution can exacerbate stress responses, disrupting gut motility and setting off an IBS event.
AIR QUALITY

IBSyncrasy
Every IBS is unique
Equally elusive is air quality. Air pollution, a pervasive problem in urban areas, can lead to systemic inflammation. It is likely that air pollution may exacerbate systemic inflammation and cause oxidative damage to the colonic mucosa, which contributes to the occurrence of IBS symptoms.
SHIFT WORKING

IBSyncrasy
Every IBS is unique
Shift work leading to irregular sleep patterns can also upset your gut. Our gut follows a circadian rhythm, with our bowel habits having their own natural pattern. When we disrupt this, like by staying up late for shift work, it can negatively impact our gut motility, and lead to irritable bowel syndrome symptoms.
TEMPERATURE EXTREMES

IBSyncrasy
Every IBS is unique
Furthermore, you might have noticed your IBS getting worse in extreme temperatures. Both prolonged exposure to cold or hot temperatures can disrupt the gut’s natural balance. In the case of a cold, it can increase vascular resistance in the gut, causing a constriction of the blood vessels and a potential IBS episode.
HIGH ALTITUDE AND CABIN PRESSURE

IBSyncrasy
Every IBS is unique
As for high altitudes, low oxygen levels can upset the gut’s oxygen balance, which may also play a part in IBS. The atmosphere within an aircraft cabin, made up of various elements, can directly impact digestive processes, potentially causing sensations like nausea. These factors include the cabin pressure, oxygen levels, and the experience of movement or vibrations. Research has indicated that the cabin pressure accessible during a typical flight altitude may substantially slow down the process of stomach emptying. This can result in symptoms similar to indigestion, particularly when coupled with a meal rich in fiber.
Knowing the trigger of the flare-up is crucial for managing IBS symptoms

IBSyncrasy
Every IBS is unique
Knowing the true instigator behind your experience of IBS flare-ups can prove pivotal in improving your quality of life. It’s not just about reacting to discomforting symptoms as they arise, but about understanding what sets off these unsettling episodes. This insightful understanding helps to create a proactive plan to preemptively handle these situations. Be it certain foods, stressors, or hormonal changes, identifying these root causes can transform the way you manage your IBS, giving you the confidence to lead a less restricted life.
Emmelia's case (a spring-IBS story)

IBSyncrasy
Every IBS is unique
Emmelia came to my office, weary and frustrated, due to her recurring bouts of abdominal pain, bloating, and unpredictable bowel habits. Her discomfort had become a significant part of her life, worsening during the spring. Given the seasonal pattern of her IBS attacks and her report of heightened reactions to certain foods, I suspected a connection to mast cell destabilization (heightened during the spring season).
Emmelia's road to relief

IBSyncrasy
Every IBS is unique
To confirm this, I recommended specialized tests such as serum tryptase and urinary N-methylhistamine, both of which are considered biomarkers of mast cell activation. The results supported our hypothesis: her mast cells were indeed more reactive, contributing to her IBS discomfort.
Guided by these findings, we initiated a therapeutic approach using natural mast cell stabilizers and unique anti-histamine probiotics. This helped to tame her mast cell activity and control the excessive histamine release. We also tailored a diet plan for Emmelia. This was a very low-histamine Mediterranean-style diet that included plenty of fresh fruits and vegetables, lean proteins, and healthy fats, but excluded high-histamine foods like fermented products, citrus fruits, and processed foods.
SIX WEEKS FOLLOW-UP

IBSyncrasy
Every IBS is unique
Six weeks later, Emmelia reported a noticeable decrease in her IBS-related pain and discomfort. The combination of natural treatments, the specific probiotics, and her new low-histamine Mediterranean diet provided a more balanced and controlled gut environment. This not only improved her IBS management but also positively impacted her overall well-being.
FAQ
What is an IBS flare-up and how long can it last?
An IBS flare-up refers to a sudden increase in symptoms of Irritable Bowel Syndrome (IBS) that can last anywhere from a few hours to several weeks. The duration of a flare-up varies depending on the individual and the specific factors that triggered the episode.
What are the common symptoms of an IBS flare-up?
Common symptoms of an IBS flare-up include abdominal pain or cramping, bloating, gas, diarrhea, constipation, or a combination of both. These symptoms can vary in intensity and duration based on the individual and the severity of the flare-up.
What factors can trigger an IBS flare-up?
Triggers can vary from person to person, but common factors that can trigger an IBS flare-up include stress, certain foods or drinks, hormonal fluctuations, and changes in routine or sleep patterns. Identifying and avoiding personal triggers can help manage and prevent flare-ups.
How can I determine my personal triggers for an IBS flare-up?
To determine your personal triggers, it’s helpful to keep a detailed food and symptom diary. Track what you eat, your stress levels, and any changes in your routine or sleep patterns, along with your IBS symptoms. Also, taking the IBSyncrasy quiz may assist you identify potential triggers.
Can stress be a factor for an IBS flare-up duration?
Yes, stress can be an aggravating factor in both the occurrence and duration of an IBS flare-up. Besides stress is a hormonal signal of a threat, either physical or psychological, and stress hormones such as epinephrine and cortisol have a direct effect on gut motility and secretory capacity.
What treatment options are available for managing an IBS flare-up?
Treatment for managing an IBS flare-up depends on the individual and the specific symptoms experienced. Common treatment options include changes in diet, stress management techniques, over-the-counter medications, and prescription medications.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.