C-section, the gut microbiome & your infant's allergies and asthma
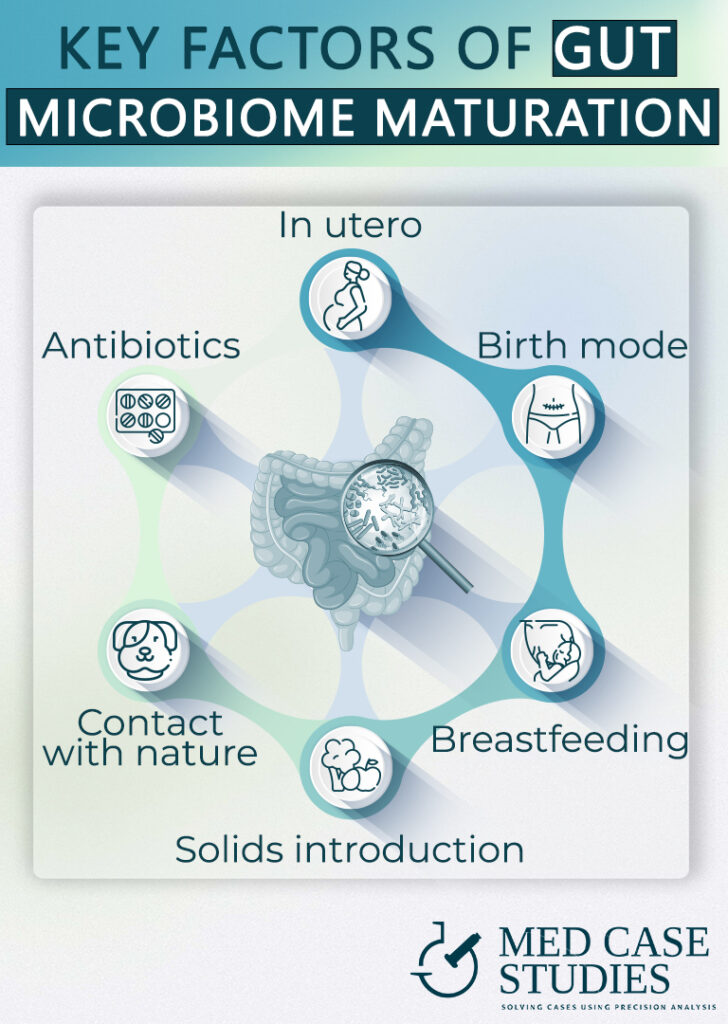
The moment of birth can shape your baby’s future health in unexpected ways. The interplay between delivery mode, the infant microbiome, and allergic disorders, through the perspective of the microbiome, highlights the critical role our earliest moments play in lifelong immune health
Can mode of birth influence the development of allergies and asthma?

IBSyncrasy
Every IBS is unique
The short answer is yes, these minutes that it takes for your baby to pass through the vaginal canal are crucial and inoculate the first and most critical batch of microbes, that will eventually grow to be their gut microbiome.
The mode of birth has been under scientific scrutiny for its potential effects on the development of allergies and asthma. Notably, a meta-analysis published in Clinical & Experimental Allergy, found a significant correlation between c-sections and an increased likelihood of food allergies and asthma in children. Since then, more than 20 studies have linked delivery mode with atopic predisposition.
The hypothesis behind these findings is rooted in the crucial early-life interaction between an infant and their mother’s microbiota. During vaginal birth, infants are exposed to a rich array of bacteria in the birth canal, forming the first “load” of commensal bacteria and playing a vital role in immune system development. This microbial exposure is largely absent in babies born via c-section, which may potentially skew the maturation of the infant’s immune system, leading to a higher risk of developing atopic conditions.
The complexity of allergy and asthma development

IBSyncrasy
Every IBS is unique
However, the relationship between birth mode and the development of asthma and allergies isn’t entirely straightforward. Some studies have not found a causal link between cesarean section birth and these conditions. Factors like genetic predisposition, environmental influences, or early life antibiotic use also hold significant sway in whether children develop food allergies or other atopic manifestations.
It is becoming evident that the complexity of this relationship is vast. It’s not merely about the mode of birth, but also about the intricate interplay of numerous factors that shape our health from the earliest stages of life. In this tangled web of factors, there’s one factor that outnumbers others – about 100 trillion of them, in fact: the gut microbiota.
The birth process and its impact on babies' gut microbiome
The acquisition of gut microbiota during birth

IBSyncrasy
Every IBS is unique
it is crucial to understand that this ecosystem starts forming at birth. While in utero, babies rely heavily on their mother’s immune system. Their own gut microbiota is relatively sparse, as shown by analyses of meconium, the baby’s first stool. Some microbial colonization does occur in utero, primarily from the mother’s urogenital tract during fertilization and conception. However, the main batch of microbes that will populate and shape the newborn’s flora for years to come is acquired during the passage through the mother’s birth canal.
The lips and tongue of the newborn play a central role in this bacterial transfer, sampling and ingesting the rich microbial communities present in the vaginal canal. This is why it’s vital for the vaginal environment to be free of pathogenic infections during and right before labor. The process of acquiring these microbes also kickstarts the baby’s immune tolerance to antigens.
The impact of delivery mode on the infant microbiome

IBSyncrasy
Every IBS is unique
The mode of delivery can significantly influence this initial microbial colonization. Children born vaginally are exposed to a different set of microbes than those born by c-section. Cesarean-section babies may acquire a different initial batch of microbes, often from the hospital environment, rather than the mother’s vaginal microbiota. This change in the initial microbiome could potentially influence the baby’s immune development and future health.
Several studies have underscored these differences, showing distinct initial microbiomes between babies born through different modes of delivery. This discovery has sparked further research into understanding the role of c-section delivery in potentially skewing the gut microbiota and the associated health outcomes.
What makes C-section babies more prone to developing asthma and allergies?
Differing immunoglobulin E and histamine release

Eating behaviors and the gut microbiome
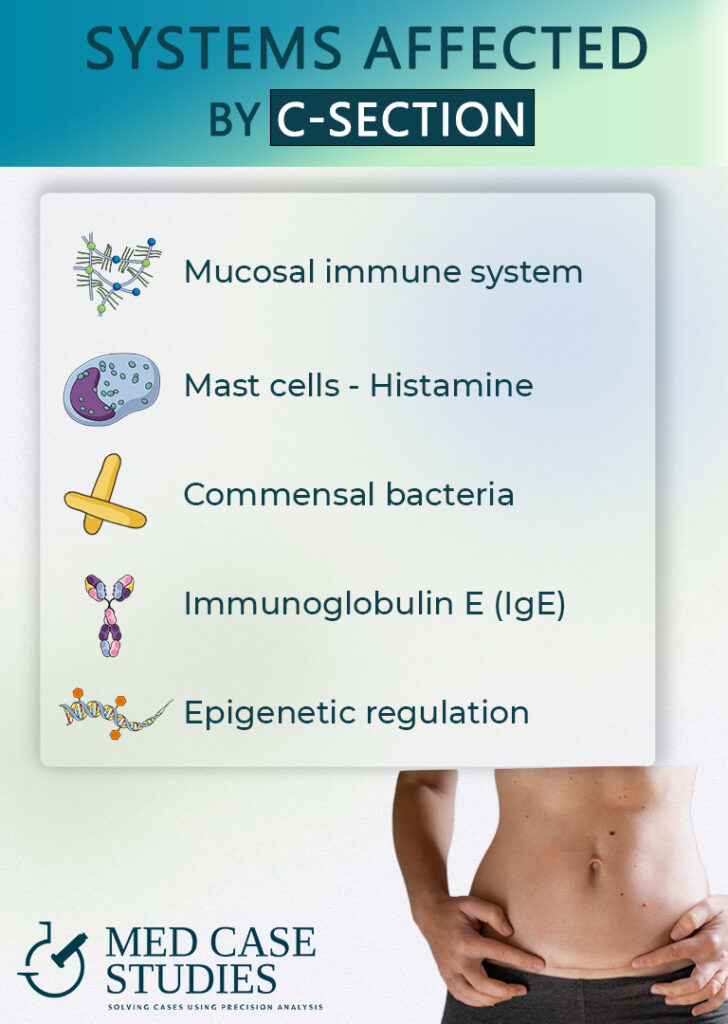
One reason for the increased susceptibility to allergies and asthma in babies born via cesarean delivery pertains to the body’s immune response. A study about the impact of c-section on allergen-specific IgE found that babies delivered this way, when exposed to common home allergens like dust and pet dander at six months old, were more likely to develop specific allergies by age two compared to those born via vaginal delivery.
In addition to this, babies born by cesarean section can have elevated histamine levels. Histamine, a compound involved in local immune responses, is associated with itching, wheezing, and allergic reactions. Interestingly, much of our body’s histamine load stems from bacterial processes in the gut, where bacteria such as Klebsiella convert the amino acid histidine into histamine. A 2015 study found that babies born via cesarean section had significantly more Klebsiella and fewer beneficial Bifidobacterium in their gut, potentially leading to higher histamine production and predisposition to allergies.
Impact on gut microbiota, immune system, and gene expression

Eating behaviors and the gut microbiome
Thirdly, the early establishment of gut microbiota can significantly impact a baby’s health during the first year of life and beyond. Babies born by ceasarean section are more likely to have a gut microbiota that lacks diversity and richness, which can potentially influence immune system development and increase the risk of atopic diseases.
Fourthly, cesarean delivery can affect the infant’s immune system directly. The lack of exposure to the maternal microbiota from the vagina may limit the stimulation and development of the infant’s immune system, making it less capable of managing allergic responses effectively.
Finally, epigenetic changes, alterations in gene activity without changes to the DNA sequence itself, may also play a role. There is emerging evidence that the mode of delivery can influence gene expression in infants, particularly genes involved in immune function and inflammation, thereby possibly increasing the propensity for developing atopic diseases.

Is IBS relevant for babies born via c-section? A case study
Linking caesarean section, IBS, and atopic conditions
Post Infectious IBS
Success case study
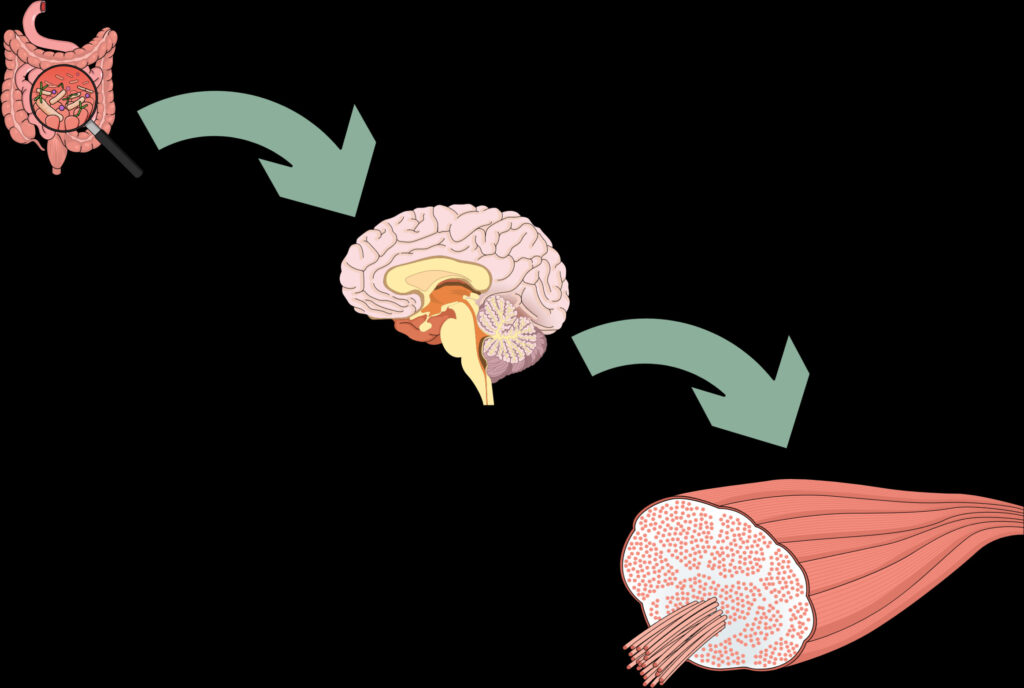
Within the atopic context, one condition that warrants discussion is Irritable Bowel Syndrome (IBS). Emerging evidence suggests a plausible connection between IBS and children born via caesarean section. IBS is increasingly recognized as a disorder influenced by the gut microbiota, with several atopic molecules, such as histamine, mast cells, and immunoglobulin E (IgE) playing significant roles in its manifestation. Additionally, serotonin a neurotransmitter that helps regulate gut motility has been heavily implicated.
It’s well-known that the initial microbiota established during labor plays a critical role in the development of a child’s immune system. Therefore, the different microbial colonization in babies born by caesarean section compared to those from natural birth can potentially contribute to the risk of food sensitization and other atopic conditions like IBS. A causal link between caesarean section and such conditions seems increasingly plausible, particularly considering that probiotics, which help restore a healthy gut microbiota, are often used to treat conditions like infantile colic.
A case study: Treating atopic symptoms and colics with probiotics
Let’s consider the case of a nine-month-old baby girl, Amelia. Amelia was born via caesarean section and began showing atopic symptoms like skin rashes and signs of allergies, along with persistent colics. The pediatrician I work with, recognizing the potential link between her symptoms and her birth mode, suggested a course of probiotics designed for infants. In addition, Amelia’s mother also took a potent probiotic blend containing mostly anti-histamine strains.
Over the next 40 days, Amelia’s mother reported a significant reduction in colics. Impressively, her atopic symptoms also started to fade. By the end of the treatment course, Amelia was colic-free, and her skin had cleared up.
How to reduce the risk of asthma and allergies in c-section babies?
Some practices that seem to optimize a baby’s microbiome after c-section are:
- Extended breastfeeding beyond 6 months
- Infantile probiotics (with caution)
- Maternal consumption of diverse and seasonal diet
- Maternal consumption of probiotics and prebiotics
- Vaginal seeding (with caution)
- Exposure to a diverse variety of seasonal vegetables upon solid introduction
- Hugging them a lot (really)
Improving microbiome and reducing atopy risk

Breastmilk is updated between feedings
- Extended breastfeeding beyond 6 months: Breast milk provides essential nutrients and immune factors that can help balance the gut microbiota in children born by c-section. A study published in JAMA Pediatrics found that exclusive breastfeeding for six months or longer was associated with a decreased risk of asthma development in a child.
- Infantile probiotics (with caution to avoid ecological homogenization): Administering carefully selected probiotics to infants can enhance their gut microbiota, reducing the risk of atopic conditions. However, it’s crucial to use diverse strains to avoid ecological homogenization, which could limit microbiome maturation and this is why giving c-section babies probiotics should be done cautiously.
- Maternal consumption of diverse and seasonal diet: A varied diet can promote a healthier gut microbiota for both the mother and child. Consuming a diverse range of foods can lead to a more robust, well-rounded microbial community, helping to reduce the risk of atopic conditions.
- Maternal consumption of probiotics and prebiotics: Probiotic and prebiotic consumption can positively influence the gut microbiota of pregnant women, impacting their babies’ microbial composition. A balanced gut microbiota during pregnancy can help mitigate the risks associated with c-section births.
Additional strategies for reducing atopy risk
- Vaginal seeding (with caution because it is not well-established): This controversial practice involves swabbing the newborn with vaginal fluids from the mother to introduce beneficial bacteria. While some studies suggest potential benefits, more research is needed to establish the safety and efficacy of this procedure.
- Exposure to a diverse variety of seasonal vegetables upon solid introduction: Introducing a wide range of vegetables to a child’s diet can help establish a diverse gut microbiota, potentially reducing the risk of atopic conditions. A study published in the Journal of Allergy and clinical Immunology found that a higher intake of fruits and vegetables during the first year of life was associated with lower asthma risk. If you pump milk or if you use baby formula, you can ask your pediatrician to include diverse vegetables and fruits to make it even healthier.
- Hugging them a lot (really): Physical contact can contribute to the transfer of skin and environmental microbes, promoting a more diverse microbiome in infants. This natural method of microbial exposure can help build a stronger immune system and reduce the risk of developing allergies. In addition, oxytocin, the hormone secreted when the baby feels safe in contact with the paternal and maternal bodies, leads to rearrangement and optimization of the gut microbiome.
FAQ
Is there a higher chance for babies born through C-section to develop allergies?
Yes, numerous peer-reviewed studies have established a link between caesarean section birth and a higher likelihood of developing allergies.
Does a C-section birth have an impact on the baby's microbiome?
Indeed, a C-section birth does impact a baby’s microbiome, resulting in differences when compared to babies born naturally.
How does a C-section birth affect the microbiome of a newborn?
A C-section birth can affect the diversity and quality of a newborn’s microbiome. For instance, histamine-producing bacteria like Klebsiella pneumoniae are found in much higher concentrations in C-section babies.
How can we replenish the microbiome after a baby is born via C-section?
The microbiome of a baby born via C-section can be replenished through extended breastfeeding, the use of probiotics and prebiotics, introducing a diverse diet upon the commencement of solid foods, and avoiding unnecessary use of antibiotics.
Is there any connection between a C-section birth and the baby's immune system?
Yes, there’s a connection between a C-section birth and a baby’s immune system. The first inoculation of microbes, which primarily primes the immune system, is influenced by the mode of delivery, thereby impacting the immune system’s maturation and tolerance.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.