The infant microbiome of breast milk vs formula
Most parents, like you, probably know the importance of the infant microbiome as a complex community of microbes inhabiting an infant’s digestive tract, including bacteria, fungi, and viruses. Beginning at birth, and especially during the first year of life, this dynamic ecosystem undergoes significant changes as it is shaped by various environmental factors, dietary inputs, and host genetics.
Understanding the infant microbiome
Why is it so crucial?

IBSyncrasy
Every IBS is unique
The first thing that comes to mind when you hear about the microbiome is that it plays a pivotal role in the early development of the immune system, as gut microbes interact with immune cells to train them to distinguish between harmful and harmless entities. For instance, certain beneficial bacteria, such as Bifidobacterium and Lactobacillus species, stimulate the production of immunoglobulin A (IgA), a type of antibody that plays a crucial role in mucosal immunity. This interaction aids in the maturation of the infant’s immune system, helping them defend against potential pathogens.
Additionally, the infant gut microbiome influences cognitive development and mental health. The gut microbiota can modulate the levels of neurotransmitters, such as serotonin and dopamine, in the brain, indicating a “gut-brain axis”. Although human studies are still in their infancy, it is speculated that similar mechanisms may occur in human babies, potentially influencing mood, behavior, and cognitive function.
The infant microbiome and long-term health

IBSyncrasy
Every IBS is unique
The development of the infant gut microbiota is determined by various sources. Initial colonization occurs during birth, with microbes from the mother’s vaginal or skin microbiome being transferred to the newborn. Following birth, the infant microbiome continues to diversify and mature through exposure to the mother’s skin, the environment, and dietary inputs including breast milk or infant formula. For instance, human breast milk is a rich source of human milk oligosaccharides (HMOs), which are indigestible sugars that selectively nourish specific beneficial bacteria, such as Bifidobacterium, promoting a healthy gut microbiota composition.
- 2′-fucosyllactose
- 3-fucosyllactose
- 3′ sialyllactose
- 6′-sialyllactose
- lacto-N-fucopentaose I, II, III, V
- lacto-N-hexaose
- lacto-N-neotetraose
- lacto-N-tetraose
- sialyl-lacto-N-tetraoses a–c

IBSyncrasy
Every IBS is unique
Finally, the early life gut microbiota has far-reaching implications for long-term health. Previous studies, including a large cohort study, have linked alterations in the infant gut microbiome during the first year of life with an increased risk of developing allergies, autoimmune diseases, and even neurodevelopmental disorders later in life. This underlines the importance of promoting healthy gut microbiota during infancy, which can be significantly influenced by the mode of feeding.
A tale of three feeding modes: breastfeeding, formula, and mixed
Nutritional value and influence on gut microbiome

Milk composition updates daily
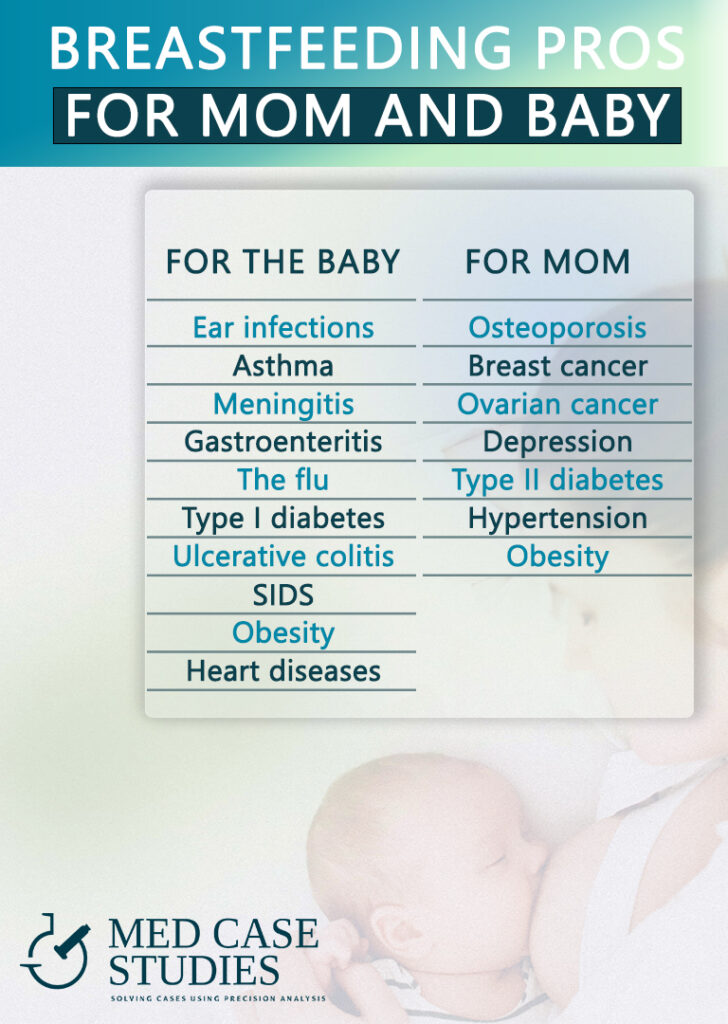
Breast milk and infant health are deeply intertwined. Thus, it’s essential to delve into the effects of the three feeding modes: breastfeeding, formula feeding, and mixed feeding. Starting with breastfeeding, it is important to understand that mothers who breast-feed their infants provide a natural diet that carries an updated composition of nutrients appropriate for an infant’s developmental stage. Breast milk is rich in growth factors, antimicrobial peptides, and proteins that support the developing immune system. Furthermore, breastfeeding supports the development of the gut, nurturing a healthy gastrointestinal microbiome characterized by high microbiota diversity and beneficial bacteria.
Formula and mixed feeding

IBSyncrasy
Every IBS is unique
Breast milk | Formula | |
|---|---|---|
Nutrition value | Breast milk provides nutrients appropriate for an infant’s developmental stage, growth factors, antimicrobial peptides, and proteins to support their developing immune system | Formula may not have the same nutritional value and benefits as breast milk |
Gut microbiome | Breastfeeding supports the establishment of a healthy gut microbiome in infants | Formula feeding can alter the gut ecology in favor of proinflammatory taxa, increase gut permeability, and increase bacterial load |
Obesity risk | Breastfeeding may reduce the risk of obesity in later childhood | Formula feeding increases the risk of obesity in later childhood |
Immunity effects | Breast milk supports the development of the infant’s immune system | Formula feeding may expose infants to proinflammatory bacteria and antigens, which could influence immune health |
Diving into the gut microbiome: Breast milk vs formula

IBSyncrasy
Every IBS is unique
A key aspect of understanding the influence of feeding modes on an infant’s health lies within the intestinal microbiota. Breastfed infants show higher levels of beneficial gut bacteria compared to those fed with formula, contributing to a healthier intestinal environment. This difference can be attributed to the myriad of nutrients, prebiotics, and probiotics found in breast milk that promote the growth of beneficial bacteria.
Yet, when it comes to microbial diversity, those fed with formula show more variation in their gut bacteria. Diversity in itself isn’t necessarily bad or good—it can depend on the types of microbes present. The microbiota development in infants can be different, and this difference is heavily influenced by their diet.
Specific bacteria and their roles

IBSyncrasy
Every IBS is unique
The dominance of specific bacteria also differs between breastfed and formula-fed infants. The intestinal microbiome in infants fed with breast milk is usually populated by Bifidobacteria and Lactobacillus species. These bacteria have been associated with positive health effects, such as enhancing the immune response and preventing the colonization of harmful bacteria. On the other hand the microbiome of formula-fed infants shows an increased relative abundance of Bacteroidetes and Firmicutes. Additionally, formula-fed infants tend to have lower levels of Veillonella and Clostridioides but higher levels of Lachnospiraceae at 3 months of age.
Antibiotic resistance is inherited

IBSyncrasy
Every IBS is unique
The early stages of life are particularly important, and the impact of colostrum, the early breast milk, shouldn’t be underestimated. It contains more lactic acid bacteria and Bifidobacterium, contributing to the initial seeding of the infant gut microbiome. This may influence the gut microbial composition later in life.
There’s also a potential concern with antibiotic resistance gene (ARG) load, which is hypothesized to be higher in formula-fed infants. Lastly, it’s worth noting that breastfed babies have a lower rate of wheezing, one of the most common reasons infants are hospitalized or receive medical care. The diverse metabolites produced by gut bacteria, which differ depending on whether infants are breastfed or formula-fed, could be a factor in these health outcomes.
How does this diversity impact the baby’s immune system and which is the role of breast milk?
The immune system and the breast milk microbiome

IBSyncrasy
Every IBS is unique
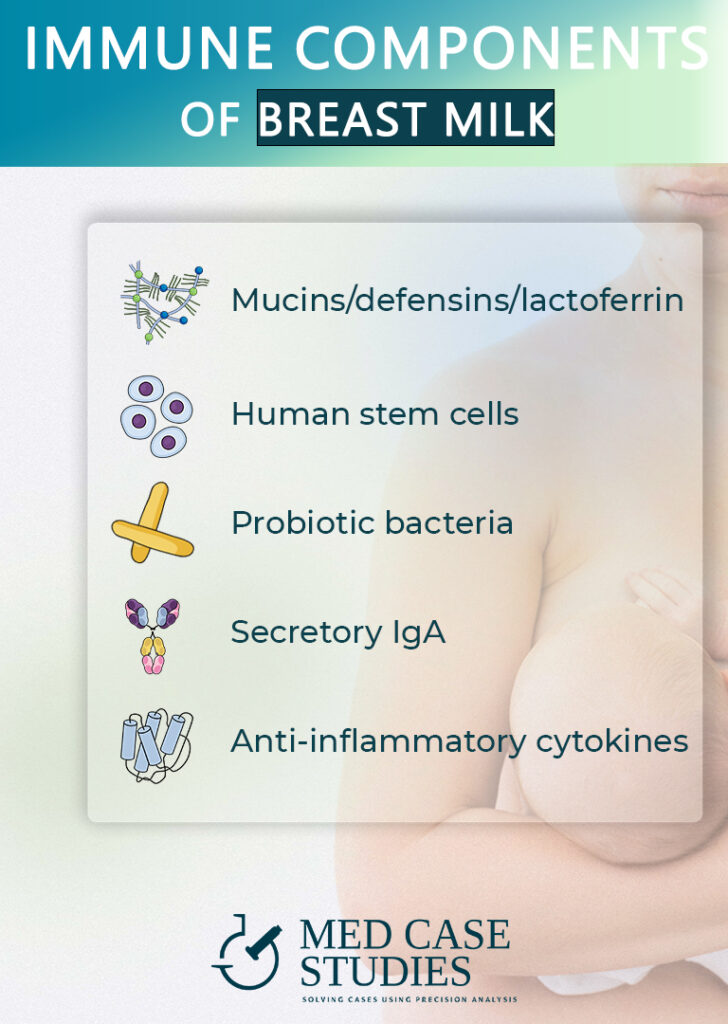
The beneficial effects of breastfeeding extend beyond basic nutrition. The microbiota in infants who are exclusively breastfed have a unique composition, which plays a significant role in establishing the initial gut environment. This initial composition is crucial for their overall health and immunity.

IBSyncrasy
Every IBS is unique
The bacteria present in breast milk facilitate the initial shift from an intrauterine Th2 prevailing response to a balanced Th1/Th2 response. This balance is essential for appropriate immune function. Furthermore, bacteria present in both colostrum and mature milk can stimulate the anti-inflammatory response, reducing the risk of various inflammatory diseases.
Breast milk microbiota and prevention of immune-mediated pathologies

IBSyncrasy
Every IBS is unique
Interestingly, the microbiota composition in children who were breast-fed and formula-fed can differ significantly. The breast milk microbiota plays a critical role in preventing immune-mediated pathologies such as asthma and atopic dermatitis. This difference underscores how breast milk may positively influence the health outcomes of infants.
Breastfeeding significantly contributes to the maturation of the infant’s immune system, impacting both local and systemic levels. This maturation can affect the gut microbiota at the genus level, leading to long-term health impacts.
Breast milk, tolerance, and protection against infections

IBSyncrasy
Every IBS is unique
Breastfeeding has been observed to have a protective role against respiratory and gastrointestinal infections, particularly between the ages of 7 and 12 months. Moreover, breast milk is crucial for establishing local and systemic immune tolerance to antigens ingested during lactation. This tolerance is key to preventing the development of allergies or autoimmune diseases.
Certain strains contained in breast milk can stimulate immunomodulatory responses, activating various immune cells like NK cells, CD4+ and CD8+ T cells, and regulatory T cells. This activation contributes to the robust immune defense in breastfed children, further establishing breast milk’s critical role in infant health.

Formula supplementation: Impact and what to do
Formula feeding can alter the composition of the gut microbiota of healthy infants, making it different from those who are primarily nourished through human milk. The intestinal environment of infants nourished by formula tends to show less Bifidobacteria species, crucial microorganisms that aid in digestion and immunity.
The diversity of gut microbiota can significantly impact the postnatal immune maturation process. Alterations in this diversity, often seen in infants who consume formula, can influence this maturation process. Furthermore, infants nourished by formula tend to have an increased incidence and/or severity of certain infectious diseases compared to their human milk-fed counterparts.
New generation formulas and gut maturation
The development of the gut microbiome can be influenced by next-generation infant formulas designed to mimic the beneficial effects of human milk on gut microbiota and the associated immune system. These formulas incorporate bioactive ingredients such as human milk oligosaccharides (HMOs), probiotics, prebiotics, and post-biotics, which can influence the gut microbiota positively.
However, supplementing infant formulas with probiotics does not raise any health concerns regarding growth, yet a few recent cases of sepsis in infants receiving probiotics have been reported. Therefore, ensuring the stability and functionality of probiotics in dairy products remains a challenge.
How to improve the gut health of a formula-fed infant?
To improve the early gut microbiota of their infant, parents may:
- Prioritize natural feeding if possible: Natural feeding is associated with a healthier gut microbiota composition and offers numerous health benefits to the baby. If natural feeding is not possible, parents should opt for a formula that closely mimics the composition of human milk.
- Select formula wisely: When natural feeding isn’t an option, parents should choose a formula that incorporates bioactive ingredients. These ingredients can help promote a healthier gut microbiota.
- Consider probiotic supplementation: Probiotics are live microorganisms that can confer health benefits when consumed in adequate amounts. Parents can consider formulas that include probiotics or provide probiotic supplements to their infants, but they should do so under the guidance of a healthcare provider.
- Avoid unnecessary antibiotics: Antibiotics can disrupt the gut microbiota. Parents should avoid giving their infants antibiotics unless it’s necessary and prescribed by a healthcare provider.
- Diversify diet: Once the infant begins eating solid foods, parents should provide a varied diet rich in fiber and fermented foods, which can help diversify and improve gut microbiota.
- Consult healthcare providers: Parents should consult with pediatricians or dietitians to make informed decisions about their infant’s nutrition and gut health.
FAQ
What are the differences between the gut microbiota of breastfed and formula-fed infants?
- Breastfed infants typically have more beneficial gut bacteria than those receiving formula.
- The gut of infants that breastfed is usually dominated by Bifidobacteria and Lactobacillus species.
- Bacteroidetes and Firmicutes are more abundant in the gut of formula-fed infants.
- The gut of infants receiving formula shows fewer Lachnospiraceae, a type of bacteria, at 3 months.
- Breast milk or formula feeding significantly influences the initial seeding of the infant’s gut.
- Association between breastfeeding and a healthier gut microbiota composition in infants is evident.
- Composition of breast milk, especially early breast milk or colostrum, heavily influences gut microbiota development.
How does the gut microbiota in breastfed babies affect their immune system?
Breast milk contains a wealth of beneficial microbes that are instrumental in shaping the infant’s gut microbiota early in life. This microbiota influences the maturation of the immune system, facilitates a balanced Th1/Th2 immune response, and stimulates anti-inflammatory processes. Breast milk also provides protection against certain infections and helps establish immune tolerance to antigens, contributing to overall health and immune function.
Are there long-term effects on the gut microbiota of babies who were formula-fed?
Research indicates that early-life formula feeding can lead to alterations in the gut microbiota in infancy. Formula-fed neonates have higher relative abundances of opportunistic pathogens and a 69% higher abundance of antibiotic-resistance genes in their gut bacteria compared to exclusively breastfed infants. This suggests that formula feeding in early life could potentially impact the gut microbiota of infants in the long term, increasing their antibiotic resistance load.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.