Acne treatment starts with gut health:
The Gut-Skin axis and the role of the microbiome

Picture this: you’ve got a big event coming up, and just like an uninvited guest, an acne breakout shows up to crash the party. We’ve all been there, right? Acne can seriously impact our self-esteem, leave behind scarring, and make us feel like we’ve tried every over-the-counter product under the sun. But what if I told you that the secret to achieving healthy skin might actually lie within your gut?
The gut-skin connection: Following the axis
The brain: The nerve centre of acne
The intricate neural networks in the brain instigate the journey of the gut-skin axis. Stress-induced signals from the brain can stimulate the production of hormones like cortisol, which disrupt the equilibrium of microbial life in the digestive tract, fostering a state of gut imbalance. This imbalance can stimulate a heightened immune response leading to widespread bodily discomfort, a key player in the pathogenesis of acne vulgaris.
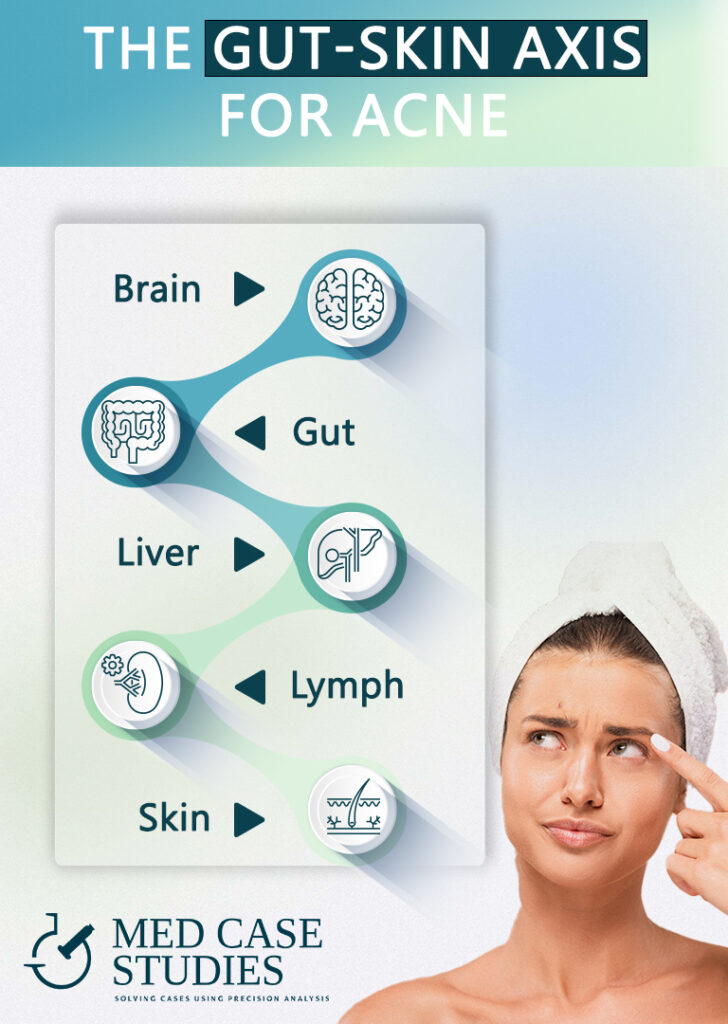
Digestive tract - The start of the axis
Next, within the digestive system, a finely tuned ecosystem of diverse microbial species exists. These microorganisms play a pivotal role in regulating the immune response and maintaining bodily harmony. A gut imbalance, however, can trigger an overactive immune response, leading to an internal state of disarray. Certain strains of microbes, when their numbers are not kept in check, can produce metabolites that incite discomfort and influence sebocytes, the cells responsible for sebum production. Excessive sebum is a major contributing factor to inflammatory acne development and other inflammatory skin disorders.
The liver: The metabolic engine
The liver, the body’s detoxification powerhouse, is closely interconnected with the gut via enterohepatic circulation. A well-functioning liver helps manage bile flow, which is vital for fat digestion and the expulsion of waste products. In acne patients, a gut imbalance can affect the liver’s ability to properly regulate bile flow, leading to a buildup of unwanted substances. These substances can accumulate in the skin, contributing to the onset of acne.
The lymphatic system: A vital conduit
The journey continues to the lymphatic system, an integral component of the immune system. The gut-associated lymphoid tissue (GALT) is the most extensive immune organ in the body, and its functioning is influenced directly by the state of the gut. An overactive immune response in the GALT due to gut imbalance can lead to widespread internal discomfort, which through the lymphatic system can lead to systemic inflammation and affect the skin.
Skin: The final destination
Finally, we reach the skin, our body’s expansive barrier, and the visible site where acne is manifest. The human skin microbiome also interacts with the gut microbiota through the gut-skin axis. An imbalanced gut, widespread internal discomfort, and a hyperactive immune response can all contribute to changes in the skin microbiome, affecting sebum production and skin homeostasis. This disruption sets the stage for acne to develop, and this is often observed in patients with acne vulgaris, as well as in people with other skin conditions.
Maria's case: Treating acne vulgaris from deep inside
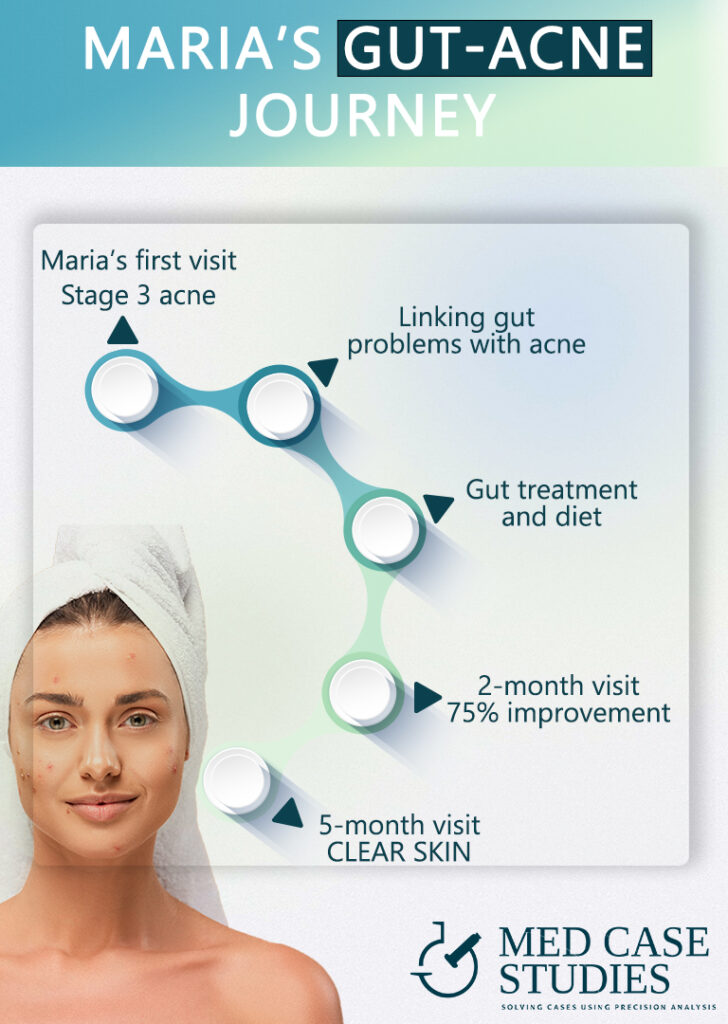
Upon meeting Maria, her condition was immediately apparent. For the past three years, she had been battling with two seemingly unrelated conditions: severe acne, and chronic Irritable Bowel Syndrome (IBS). Her facial skin, which could typically be classified as having mild to moderate acne, had escalated to stage 3, featuring inflamed cysts and nodules that rendered her complexion red and irritated. Concurrently, her chronic IBS further aggravated her quality of life.
The conventional treatment of acne vulgaris hadn’t provided Maria with any lasting relief. Recognizing that the root cause of her issues could be deeply entwined within her body’s internal ecosystem, an alternative approach was taken. She was prescribed a carefully selected mix of specific live microorganisms, mucosal nutrients, and a potent antimicrobial blend.
Dietary and lifestyle adjustments
In conjunction with the treatment, Maria was given strict dietary guidelines. For the initial two months, she was to follow a diet that was devoid of dairy and wheat products. Instead, she was to consume a variety of seasonal fruits, vegetables, and lean proteins. These changes aimed to nourish and balance her internal environment, allowing her body to better manage the external signs of distress, such as her severe acne.
A set of behavioral and lifestyle modifications were also recommended. Stress management techniques, adequate sleep, and regular physical activity were all a part of her comprehensive acne treatment regimen. These changes aimed to further harmonize the intricate relationship between her gut flora and skin microbes.
Rediscovering clear, normal skin
The results of these interventions were nothing short of astounding. Maria’s internal disturbances gradually subsided, as did the signs of distress on her skin. The inflammation and redness associated with her severe acne slowly receded, replaced by clear, normal skin. The microbiome may be complex and widely diverse, but with the right approach, it can be harnessed to treat acne and other manifestations of internal disharmony effectively. Complete resolution of Maria’s facial acne would only come after 5 months of sticking to the diet, but even after she reintroduced some dairy and wheat, her skin remained clear and acne-free.
This case reaffirms the intricate interplay between gut and skin microbiota, showing that care for one’s internal environment extends far beyond the boundaries of our gut. A balanced and nourished body echoes its well-being on the skin, offering new hope for those battling similar issues.
Gut microbial metabolites: The good and the bad
Gut microbial metabolites can have both beneficial and detrimental effects on the skin, playing a crucial role in the health and appearance of our skin.
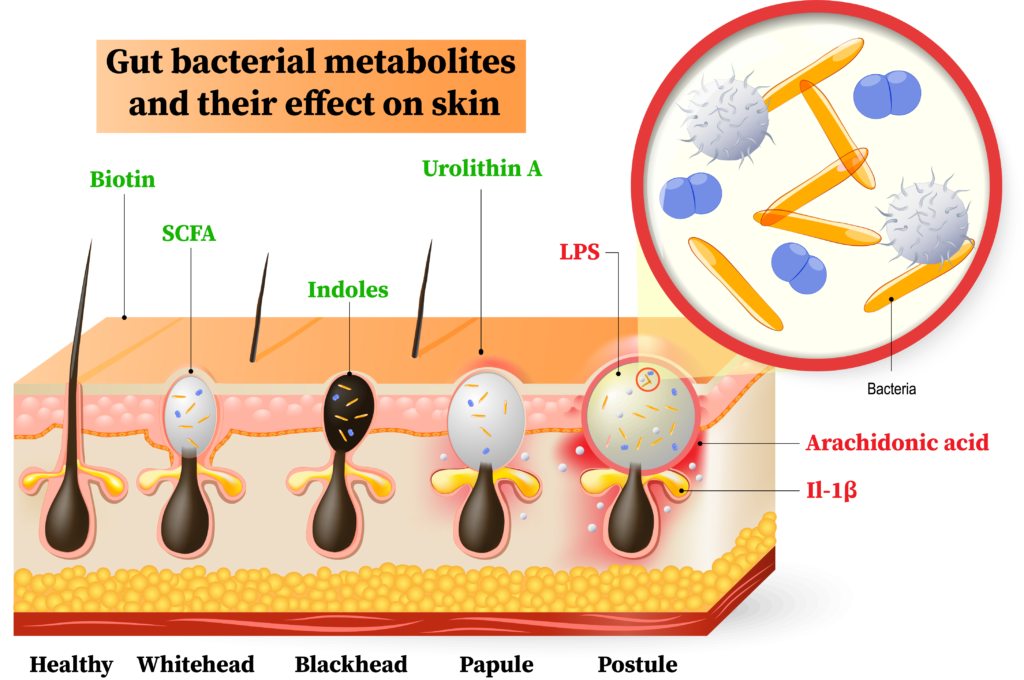
Good metabolites
Good metabolites, such as short-chain fatty acids (SCFAs) and urolithin A, contribute to maintaining a healthy skin barrier and regulating sebum production. SCFAs, produced by gut bacteria during the fermentation of dietary fibers, help maintain skin barrier function and regulate sebum production, thus preventing pimple formation. Urolithin A promotes epidermal barrier function by stimulating keratinocyte differentiation and enhancing the expression of barrier-related proteins like filaggrin and involucrin.
Bad metabolites
On the other hand, bad metabolites like lipopolysaccharides (LPS) and arachidonic acid can trigger inflammation and exacerbate acne. LPS can initiate an inflammatory response in the skin, leading to excessive production of keratinocytes, causing pores to clog and form comedones. Arachidonic acid promotes the production of inflammatory mediators like prostaglandins and leukotrienes, contributing to pustule development by causing increased inflammation and pus formation in the affected area.
Hormonal influence on gut function: How do hormones play a role?
Our gut microbiota doesn’t just dance to the beat of its own drum—it also sways to the endocrine rhythms within our body. Hormonal imbalances, such as those seen in insulin resistance and polycystic ovary syndrome (PCOS), can directly impact gut function, leading to changes in our gut ecology and exacerbating acne.
Acne-related hormone | Specific bacterial strain involved |
|---|---|
Insulin | Bacteroides vulgatus |
Testosterone | Cutibacterium acnes |
Estrogen | Lactobacillus reuteri |
Progesterone | Bifidobacterium longum |
Cortisol | Lactobacillus acidophilus |
Temporary acne relief with contraceptives: Why is it not a long-term solution?

While contraceptives can seem like a magical solution for acne, they may be just a temporary fix. The combined pill suppresses our natural hormones, replacing them with synthetic estrogen and progestogen. The estrogen in the pill reduces sebum (oil) production, which contributes to acne. However, this effect only lasts as long as you’re on the pill.
When you stop taking the pill, your body’s reproductive system goes back to normal, which can cause a resurgence of acne. This is due to rebound sebum production and a temporary surge in androgens (male hormones) as your ovaries kick back into action. Post-pill acne typically peaks about six months after stopping the pill and can last up to a year or more.
Foods that disrupt gut microbiome and aggravate acne
Your diet plays a crucial role in maintaining a healthy gut, which can have a direct impact on your skin. Certain foods are known to disrupt the gut microbiome, potentially leading to a leaky gut, skin inflammation, and aggravated acne. By identifying these culprits and adjusting your diet, you can support a healthy gut diversity and potentially reduce acne.
Sugar: Refined sugars and sweeteners in sodas, juices, and other processed foods can raise blood sugar levels, leading to increased insulin and sebum production, both associated with acne.
Dairy products: Some studies have found a relationship between acne and the consumption of low-fat and skim milk. If you notice acne after consuming dairy, consider reducing your intake.
Fast food: The link between fast food and acne is not well understood, but teenagers who consume large amounts of burgers and fries often experience skin issues.
- Greasy food: Fried foods and high-fat items like bacon and burgers can cause an outbreak of pimples due to their excess oil and fat content.
Whey protein powder: Consuming whey protein can cause skin cells to grow and multiply faster, along with raising insulin levels, both of which contribute to acne.
Refined grains: Breads, pasta, cereals, and rice noodles made with refined white flour have a high glycemic index and can raise blood sugar levels, leading to increased sebum production and faster cell growth, resulting in acne.

Prebiotics and probiotics for acne: Nurturing your gut microbiota
Several studies have explored the potential of probiotics and other treatments for acne. Jung et al. found that combining oral probiotics and antibiotics effectively reduced acne lesions and antibiotic side effects. Other research showed that specific probiotics and natural compounds, such as konjac glucomannan hydrolysates, E. faecalis SL-5, heat-killed L. plantarum-GMNL6, and Weissella viridescens UCO-SMC3, could inhibit acne-causing bacteria, reduce inflammation, and improve overall skin health. Additionally, a study involving a combination of probiotic lactic acid bacteria and Curcuma longa extract showed promising antibacterial effects against acne-causing bacteria. Topical probiotics may be a useful treatment option sometimes, but from my experience, they generally lead to temporary relief.
Researchers | Key findings |
|---|---|
Jung et al. | Synergistic effects of oral probiotics and antibiotics reduced acne lesions and minimized antibiotic side effects.
|
Al‐Ghazzewi et al. | Inhibitory effects on acne-causing bacteria, suggesting further research into their therapeutic or prophylactic use. |
Kang et al. | E. faecalis SL-5 reduced inflammation, with potential as an alternative option for future acne therapy. |
Espinoza-Monje et al. | Oral or topical administration of Weissella viridescens UCO-SMC3 favorably modulated inflammatory response and reduced acne eruptions. |
Kim, Jina, et al. | Combination of probiotic LAB and CLE produced cooperative antibacterial effects against C. acnes |
Practical tips for both gut health and acne
General tips for improving gut health and acne:
- Eat clean: Focus on whole, unprocessed foods that are rich in nutrients and fiber, which will promote a balanced gut microbial ecology.
- Avoid dairy: Dairy products can contribute to inflammation and exacerbate acne in some individuals. Consume dairy only twice per week.
- Consume fermented foods: Incorporating fermented foods like kimchi, sauerkraut, and kefir can introduce beneficial bacteria into the gut.
- Increase fiber intake: Include a salad as a side plate with every meal. Consuming a diet high in fiber from fruits, vegetables, and whole grains can help support a diverse and healthy intestinal microbiome.
- Drink plenty of water: Target 10 glasses of water daily. At least 6 of them until noon. Staying hydrated is essential for overall health and helps maintain a healthy and thriving gut environment.
- Limit sugar intake: Forget about sugar. You just need one month. Excessive sugar consumption can negatively impact the gut microbiome and contribute to acne.
- Manage stress: Stress can disrupt the intestinal microbiome and may worsen acne, so it’s important to practice stress management techniques like meditation or exercise.
Specific tips for improving gut health and acne:
- Eat before 19:00: Eating earlier in the evening can help reduce sebum production during the night. This is because the gut microbiome influences acne through its effects on sebum production, which is regulated by the skin’s circadian rhythm.
- Sleep at least 2 times per week before 23:00: Taking advantage of the full melatonin potential can help regulate the gut microbiome and promote a healthy skin surface. Melatonin, a hormone produced at night, has been shown to have anti-inflammatory and antioxidant properties that can benefit the pathophysiology of acne.
- Add prebiotic-rich foods: Consuming foods high in prebiotics, such as garlic, onions, and leeks, can help support the growth of beneficial bacteria in the gut, which may influence acne.
- Incorporate polyphenol-rich foods: Foods high in polyphenols, like berries, green tea, and endives, have been shown to support a diverse gut microbiome and may help improve acne by reducing inflammation and oxidative stress.
Practice intermittent fasting: Intermittent fasting can help regulate gut bacteria and reduce inflammation, benefiting acne-prone skin. Experiment with different fasting windows, such as 16:8 or 14:10, to find the best fit for your lifestyle.
Sip on green tea: Green tea is rich in antioxidants and has anti-inflammatory properties that can benefit gut microbial ecology and inflammatory skin diseases. EGCG, a very potent catechin of green tea has been shown to increase the diversity of the gut microbiome, an index that is linked to better skin physiology.
My experience with acne treatment
Over the years, I’ve had the privilege of overseeing more than 3,000 cases related to gut health. Interestingly, a significant number of clients (mostly young women) came to my office seeking help for gut-related issues, not even considering the potential link between their GI function and acne. As we worked together to improve their gut microbiome, a fascinating pattern began to emerge. Many clients reported not only an improvement in their gut problems but also a noticeable difference in their skin. In some cases, their acne completely vanished! This incredible correlation between gut health and acne motivated me to further investigate and understand the intricacies of the gut-skin connection. As a result, I’ve been able to help countless individuals not only restore their gastrointestinal health but also achieve clearer, healthier skin. The journey has been both rewarding and eye-opening, demonstrating the remarkable potential of addressing gut health to transform both inner wellness and outward appearance.
Take the first step towards a healthier gut and clearer skin today. Book an appointment to receive personalized guidance and support, tailored to your specific needs. Don’t hesitate to send an email for further information or to discuss how I can help you achieve your skin health goals by addressing your gut health and microbiome.
FAQ
How to improve gut health for acne?
Improving gut health for acne may include a dairy and wheat-free diet, which could initially worsen symptoms. Fasting can help reset gut flora. An antimicrobial blend may also be beneficial, reducing harmful bacteria.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.