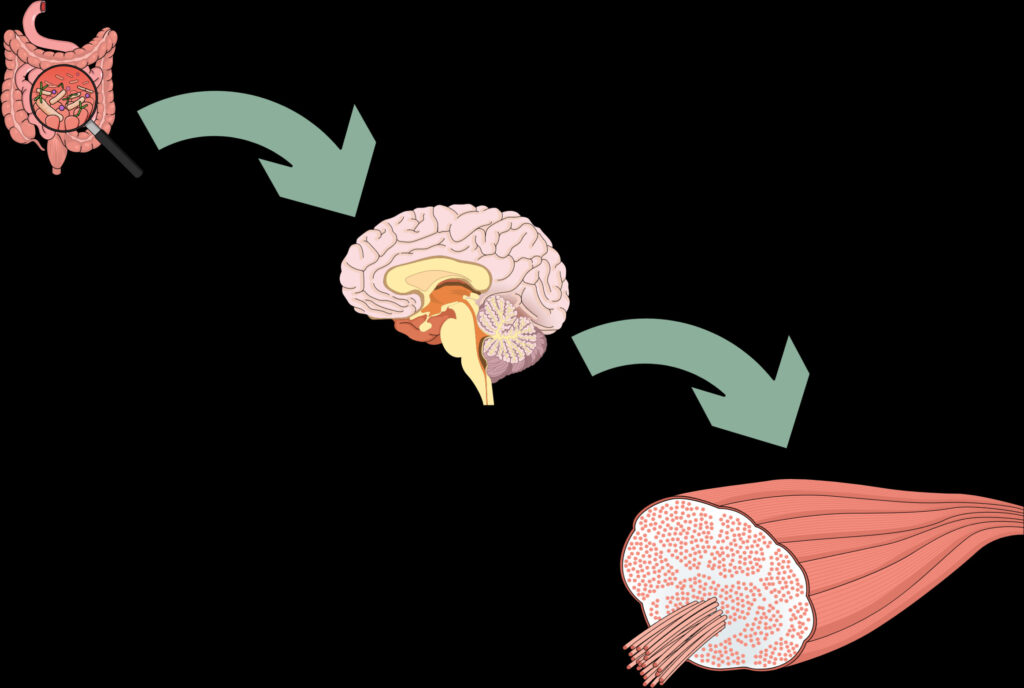
Intestinal permeability: Beneficial process or leaky gut?
The most common aspect of post-infectious IBS is a persistent increase in intestinal tight junctions ("leaky gut")
Article Highlights
Have you ever felt like the gastroenteritis you had 6 months ago seems to last forever? You might be dealing with post-infectious irritable bowel syndrome (IBS), which is closely linked to a phenomenon known as “leaky gut” or persistently increased intestinal permeability.
Is intestinal permeability a bad thing after all?
What is leaky gut?
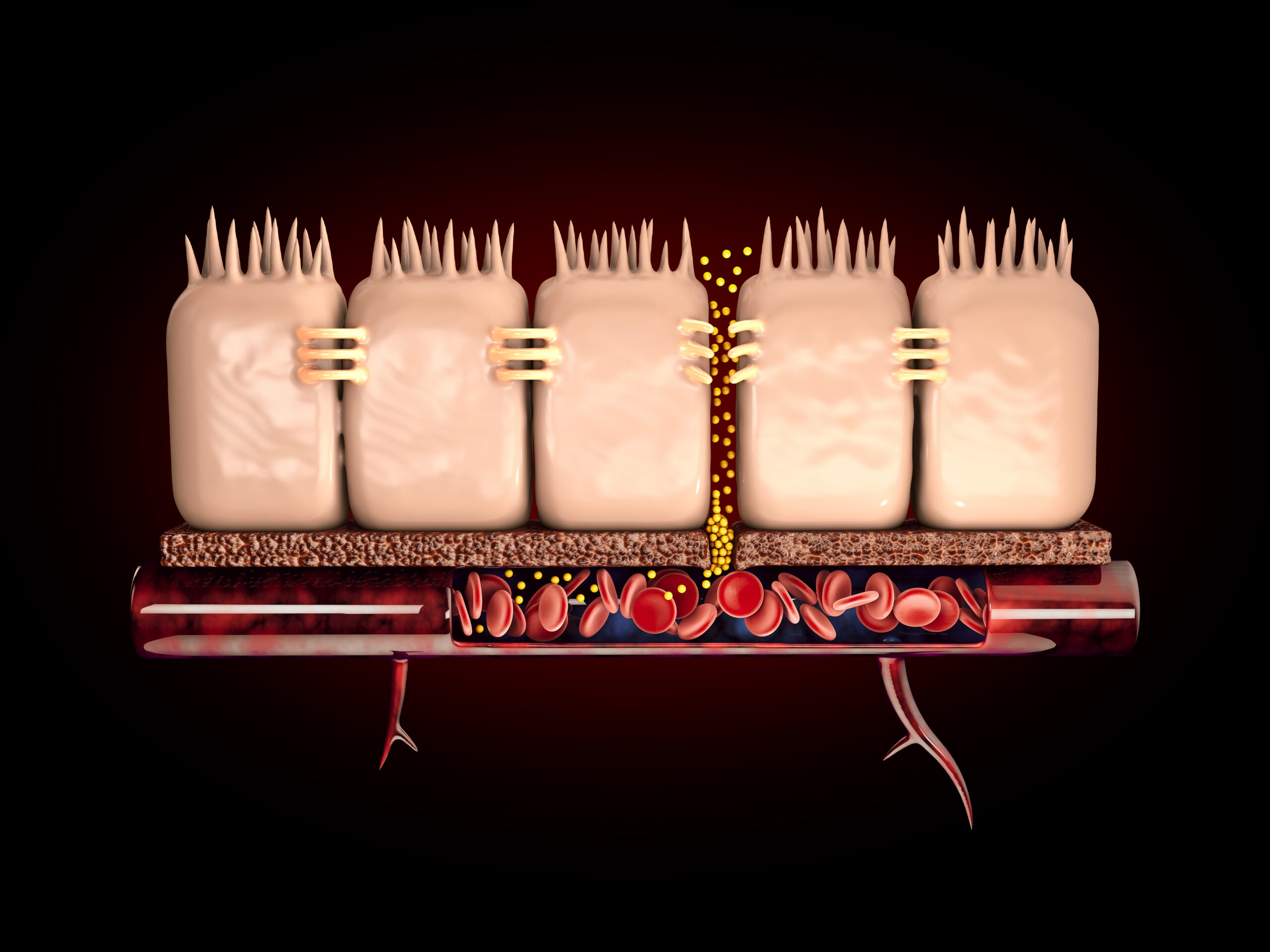
Leaky gut, also referred to as “leaky gut syndrome,” occurs when the tight junctions in the intestinal wall become compromised, allowing harmful substances like bacteria and toxins to pass into the bloodstream. This altered intestinal permeability may contribute to various health issues, including gastrointestinal disorders, autoimmune diseases, and inflammation.
The Evolutionary Benefits of Increased Intestinal Permeability During Infection
During an infection, increased intestinal permeability can be beneficial in several ways. The immune response is enhanced as the permeability allows more immune cells to access the site of infection, promoting pathogen clearance. This is particularly important in cases of gastroenteritis, where harmful bacteria or viruses are present in the gastrointestinal tract. By increasing the permeability of the intestinal barrier, the body can mount a more robust and targeted response to eliminate the infectious agents, ultimately helping to restore gut health and prevent chronic inflammation.
Mechanisms and Mediators of Increased Intestinal Permeability
The integrity of the intestinal barrier is maintained by tight junction proteins, which act as a seal between cells in the intestinal lining. When these tight junctions are disrupted, it can result in intestinal hyperpermeability or leaky gut. Several factors can contribute to this disruption, including inflammation, stress, and imbalances in gut microbiota.
Inflammatory mediators, such as cytokines and zonulin (a modulator of intercellular tight junctions), play a significant role in altering intestinal barrier function. They can increase the permeability of the gut lining, allowing harmful substances to cross the intestine and enter the bloodstream. This can trigger a cascade of immune responses and contribute to chronic inflammation, which may play a role in the development of various chronic diseases.
Post-infectious IBS and the persistent leaky gut problem
When Increased Intestinal Permeability Persists After Infection Resolution
Ideally, the gut barrier should return to its normal function after an infection has been resolved. However, in some cases, increased permeability might persist, leading to the development of post-infectious IBS. This chronic condition can cause a wide range of gastrointestinal symptoms, including abdominal pain, bloating, diarrhea, and constipation.
The Connection Between Leaky Gut and Post-Infectious IBS
Studies have shown that people with post-infectious IBS often exhibit signs of increased intestinal permeability. The persistent increased intestinal permeability after infection resolution can contribute to ongoing inflammation and imbalances in gut microbiota. Moreover, the compromised gut barrier allows for the continuous passage of harmful substances, which can lead to the activation of the immune system and exacerbation of IBS symptoms.
Reasons Why Intestinal Permeability is Not Completely Restored After Infection
Several lifestyle habits can hinder the restoration of intestinal permeability after an infection. These habits include poor food choices, such as consuming processed foods and a diet high in sugar and unhealthy fats, which can contribute to inflammatory reactions and negatively affect gut health. Late-night eating can disrupt the natural circadian rhythm of the digestive system, leading to inefficient nutrient absorption and a weakened gut barrier. Additionally, poor sleep quality can impair the body’s ability to heal, repair, and restore the intestinal lining.
Biological Explanations for the Impact of These Habits
The negative impact of these habits on the restoration of intestinal permeability can be attributed to several biological factors. Chronic inflammation, driven by an unhealthy diet and disrupted circadian rhythm, can contribute to intestinal hyperpermeability and disrupt the delicate balance of the gut microbiota. Imbalanced bacteria in your gut can lead to a host of gastrointestinal disorders, including irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD). Furthermore, poor sleep quality can weaken the immune response, making it more difficult for the body to combat lingering pathogens and fully restore gut integrity.
Other factors are:
Stress: Chronic stress can have a profound effect on gut health, as it can lead to the release of stress hormones that negatively impact the intestinal barrier function. Stress can also alter the gut microbiota, making it more difficult for the body to restore intestinal permeability to its optimal state, while it may increase the sensitivity to common allergens, like milk proteins and soya.
Environmental toxins: Exposure to environmental toxins, such as pesticides, heavy metals, and pollutants, can damage the intestinal lining and contribute to symptoms associated with intestinal permeability. These toxins can directly impact the tight junctions, leading to increased permeability and allowing harmful substances to enter the bloodstream.
Genetic predispositions: Certain individuals may have a genetic predisposition to develop leaky gut or experience difficulty in restoring intestinal permeability after an infection. Besides patients suffering from celiac disease, type 1 diabetes, or functional disorders like chronic fatigue syndrome, other genes may contribute to compromised gut barrier function. These genetic factors can influence the production of proteins involved in barrier function, immune response, and inflammatory cascades, making it more challenging for the body to achieve a balanced state of intestinal permeability.
What to do to recover from post-infectious IBS fast?
Take probiotics during and after infection
Supplementing with probiotics during and after infection can provide numerous benefits, such as immune support and maintaining gut microbiota balance. Continue probiotic supplementation for at least one week after the infection has resolved to support recovery and restoration of the intestine's barrier function.
Avoid vigorous exercise for at least 7 days after recovery
Vigorous exercise increases gut permeability. Refraining from vigorous exercise for at least a week after infection allows the body to rest, recover, and focus on healing. Intense physical activity can exacerbate intestinal permeability. Instead, engaging in gentle activities such as walking or yoga can help support stress reduction and overall well-being during the recovery process.
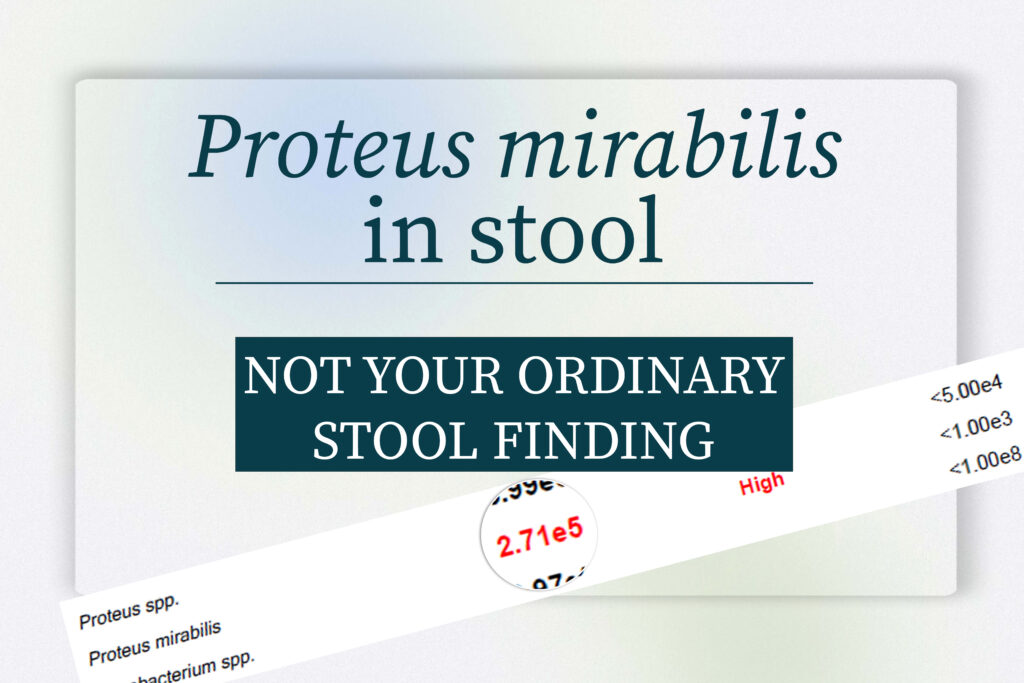
Take glutamine
Glutamine is an amino acid that supports intestinal lining health and immune function. However, it should be avoided if a Proteus urinary tract infection (UTI) is suspected, as it may worsen the condition. In other cases, glutamine can aid in restoring intestinal permeability by providing essential nutrients to the gut lining and promoting tissue repair.
Incorporate liquid dinners for at least 7 days post-infection
Consuming liquid dinners, such as soups, for at least seven days after infection can aid in nutrient absorption and ease digestion. Liquid meals are more easily broken down by the gastrointestinal system, reducing stress on the gut and allowing it to focus on healing. This approach also provides essential nutrients needed for tissue repair and immune function, ultimately benefiting the restoration of intestinal permeability.
Supplement with zinc for at least a month after infection
Zinc is an essential nutrient that plays a crucial role in immune function, tissue repair, and reducing inflammation. Supplementing with zinc for at least a month after infection can help support the restoration of intestinal permeability by promoting the healing of the gut lining and modulating immune responses.
Drink chamomile and ginger tea in the afternoon
Chamomile and ginger tea have soothing effects on the digestive system and possess anti-inflammatory properties. Drinking these teas in the afternoon can help alleviate gastrointestinal discomfort and support the restoration of intestinal permeability.

My experience
From my extensive counseling experience, I’ve observed that many individuals mistakenly treat intestinal permeability as a disease in itself, instead of addressing the underlying causes. As a telltale sign of systemic imbalances, increased intestinal permeability is a symptom rather than the root issue. While it is normal for tight junction gaps to increase during infection, addressing and treating this permeability after infection resolution is vital to prevent long-term symptoms, particularly within the context of post-infectious IBS.
Hall, Emily H., and Sheila E. Crowe. “Environmental and lifestyle influences on disorders of the large and small intestine: implications for treatment.” Digestive Diseases 29.2 (2011): 249-254.
Thabane, Marroon, and John K. Marshall. “Post-infectious irritable bowel syndrome.” World journal of gastroenterology: WJG 15.29 (2009): 3591.
Piche, T. “Tight junctions and IBS‐the link between epithelial permeability, low‐grade inflammation, and symptom generation?.” Neurogastroenterology & Motility 26.3 (2014): 296-302.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.