Breast milk and bacteria
Upgrading the infant microbiome

Breastfeeding is a dynamic process
Breast milk serves as more than merely a nutritional source for infants – it is also crucial in shaping the development of the infant microbiome. Human milk oligosaccharides (HMOs), a specific carbohydrate found in breast milk, have been demonstrated to influence the composition and function of the gut microbiota during the first year of life, thereby altering developmental trajectories. HMOs are not digested by the infant but are fermented by bacteria in their large intestine, resulting in the production of short-chain fatty acids with numerous health benefits. By fostering the growth of good bacteria and suppressing the proliferation of harmful bacteria, HMOs may contribute to the promotion of a healthy microbial community in the infant’s gut. This, in turn, can positively affect the infant’s overall health and development.
Which are the roles of the microbiome?
The microbiome is diverse and unique to each individual, with various factors such as diet, environment, and genetics influencing it.
Some vital roles of the microbiome during the first year of life related to health include:
- Digestion: The commensal bacteria are essential in food digestion and nutrient absorption. They assist in breaking down complex sugars and fibers that the body cannot digest independently and produce specific vitamins, such as vitamin K and B-vitamins.
- Immunity: The microbiome contributes to the body’s protection against illness and infection by generating antimicrobial substances and activating the immune system. It also helps to inhibit the overgrowth of harmful bacteria and other microorganisms.
- Metabolism: It influences metabolism by affecting the production and breakdown of particular hormones and chemicals in the body. It has also been associated with the development of obesity and other metabolic disorders.
- Mental health: Specific microbial populations have been linked to mental health and connected to conditions like depression, anxiety, and autism.
- Allergies and asthma: The absence of pathogenic bacteria early in life confers a reduced risk of developing allergies and asthma.
- Skin health: Epidermal bacteria play a role in maintaining skin health by protecting against infections and influencing the production of oils and other substances that keep the skin hydrated and healthy.
- Postbiotics: Postbiotics are metabolic byproducts generated by healthy intestinal bacteria that offer various health benefits. For instance, specific postbiotics have anti-inflammatory effects and have been associated with preventing certain diseases.
- Neonatal development: It is crucial in newborn development, especially during the first few months of life. A healthy gut microbial ecology can support growth and development and lower the risk of certain health issues.
The breast milk microbiome: Inoculating the baby's ecology
Besides its well-known nutrients, breast milk also contains a diverse array of beneficial microorganisms, mostly bacteria, that can help to shape the infant microbiome. Human breast milk was once considered sterile, but it is now known to contain commensal and probiotic bacteria such as Lactobacillus fermentum and Lactobacillus gasseri. It contains approximately 1000 colony-forming units of various bacterial species per milliliter, and infants receive around 800,000 bacteria from breast milk each day.
The infant microbiome begins developing in utero but is largely influenced by the environment after birth through mechanisms such as vaginal flora during delivery and after. Breastfeeding is a key factor determining the composition and diversity of the infant gut microbiota, and the gut microbiota of breastfed infants is typically more diverse than that of formula-fed infants. Breast milk contains various bacterial species. Some strains isolated from breast milk include Staphylococcus, Streptococcus, Bifidobacterium, Lactobacillus, and Enterobacteriaceae, and the composition of human milk microbiota can vary based on factors such as lactation stage and the mother’s diet and lifestyle. Colostrum, the initial breast milk produced after childbirth, contains a more diverse number of bacterial species than transitional or mature milk. This diversity of bacteria in colostrum can help establish and shape the infant’s gut microbiota during the critical early stages of life.
Breast milk also contains prebiotics
Besides well-known nutrients and commensal bacteria, mothers’ milk also contains prebiotics, which are non-digestible compounds that feed and support the growth of good bacteria in the infant’s gut. Prebiotics play a crucial role in supporting the development and maintenance of healthy bacteria in a baby’s intestinal environment and have been linked to a range of health benefits in infants and adults.
- Oligosaccharides: Complex sugars resistant to digestion, serving as a food source for beneficial gut bacteria.
- Healthy fats: Breast milk contains various fats, including short-chain fatty acids, which exhibit prebiotic effects and support the growth of good bacteria in the gut.
- Lactoferrin: A protein in breast milk that has prebiotic effects and supports the growth of beneficial gut bacteria.
- Epidermal growth factor: A protein in breast milk that has prebiotic effects and supports the growth of good bacteria in the gut.
- Lysozyme: An enzyme in breast milk that has prebiotic effects and supports the growth of beneficial gut bacteria.
Breast milk provides protection from several health conditions
Breastfeeding has been associated with a decreased likelihood of several health issues in mothers, infants and children. Some of the health conditions linked to breastfeeding include:
- Cancer risk: Nursing for at least 6 months is linked to a lower risk of certain cancers, including breast and ovarian cancer.
- Enhanced bone health: Lactation can also improve bone density, reducing the risk of osteoporosis in mothers.
- Weight loss facilitation: It helps mothers lose weight and return to their pre-pregnancy weight more quickly.

Pediatric IBS
Case study
- Reduced gastrointestinal symptoms: Breastfed babies exhibit a reduced risk of presenting with functional bowel symptoms, like bloating, diarrhea, constipation, and IBS.
- Allergies: Lower risk of developing allergies, such as food allergies and eczema.
- Asthma: Reduced likelihood of developing asthma and other respiratory conditions.
- Obesity: Lower risk of developing obesity and other metabolic disorders.
- Infections: Decreased risk of certain infections, including respiratory tract infections, ear infections, and gastrointestinal infections.
- Sudden Infant Death Syndrome (SIDS): Breastfeeding is associated with a reduced risk of SIDS and other forms of infant mortality.
What factors influence gut microbiota shaping?
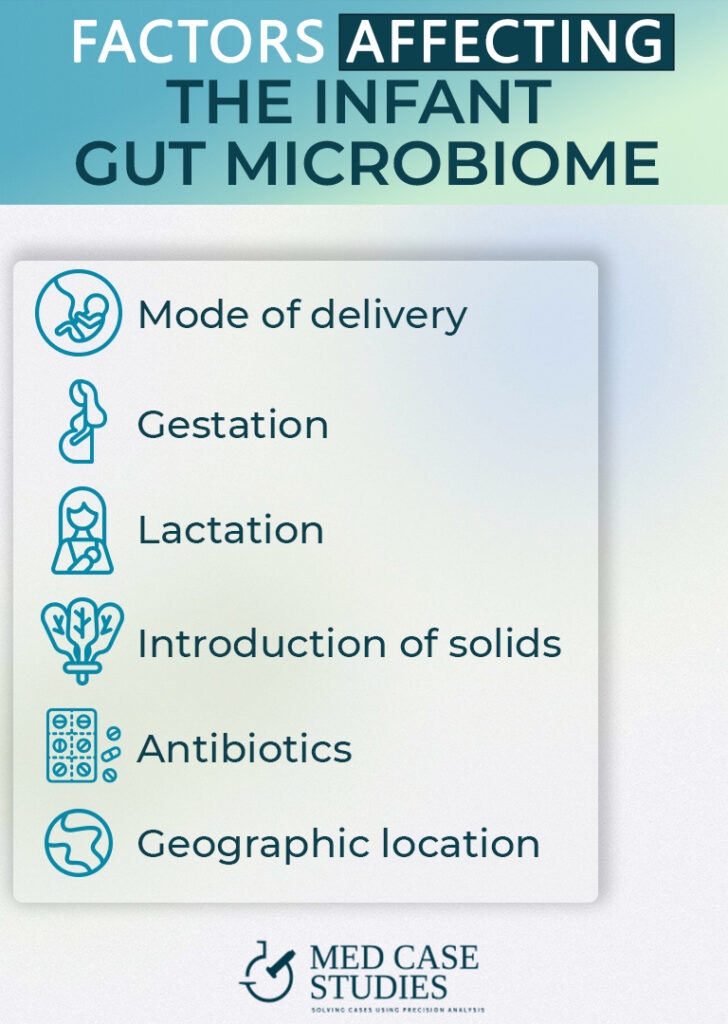
The microbiome of the baby begins to develop in utero but is significantly influenced by the environment after birth. Consequently, a baby’s overall gut microbiota composition is affected by various factors such as diet, environment, mode of delivery, and other exposures.
- Gestation: During pregnancy, the developing fetus is exposed to bacteria and other microorganisms from the mother’s microbiome, which can influence the infant gut microbiota composition.
- Mode of delivery: Infants born via cesarean section may have a different initial microbial populations than those born vaginally, as they are exposed to different types of bacteria during delivery.
- Breastfeeding: Lactation plays an essential role in shaping the child’s microbiome. Milk microbiome composition exhibits a vast variation that supports the development of a healthy microbiome in infants. Formula-fed infants may have a different initial microbial batch than breastfed infants, as the formula lacks the same types of lactic acid bacteria and prebiotics found in breast milk.
- Introduction of solids: The age at which solids are introduced can also influence the baby’s gut microbiome development. Introducing solids earlier or later than recommended may alter the types of bacteria present in the infant microbiome.
- Antibiotics: Antibiotic treatments can also change the percentage of beneficial live bacteria, as they can kill both harmful and beneficial microorganisms.
- Geographic location: Different regions of the world have different bacterial exposures and exposure to various types of bacteria can affect a child’s microflora.
Children update milk composition through saliva
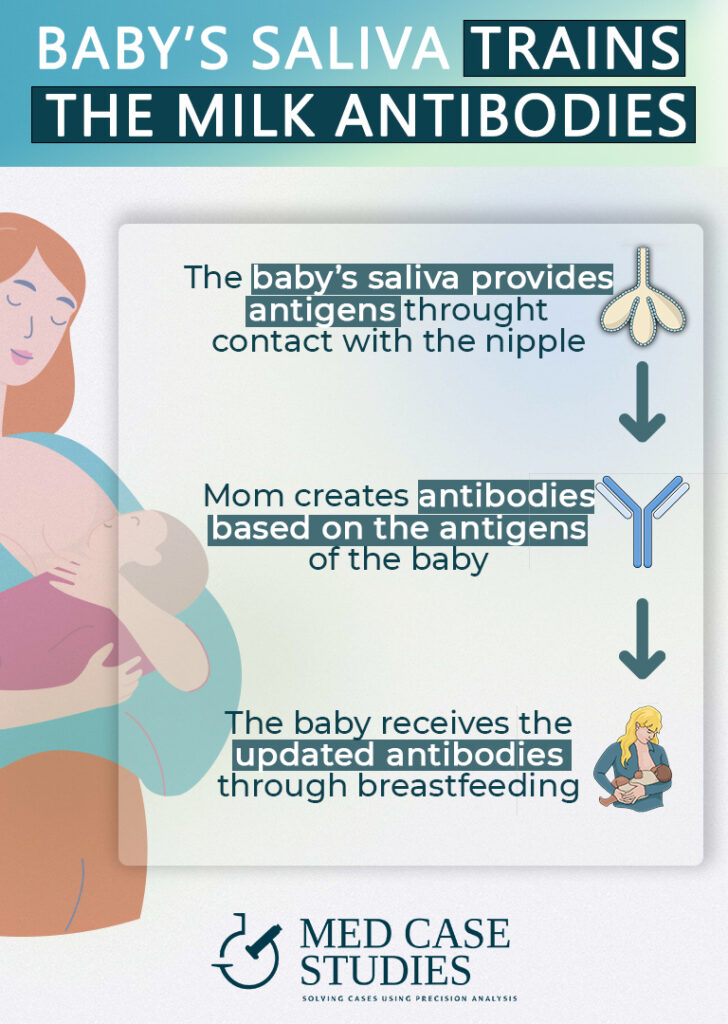
Breastfeeding is a dynamic process with various factors influencing the composition of breast milk. Interestingly, children contribute to updating the milk composition through their saliva when they touch the nipple with their lips, helping introduce new bacteria to the milk and the infant’s microbiome. This is why pumped breast milk may have less updated and diverse bacterial populations than milk nursed directly at the breast.
Saliva is a complex fluid containing a diverse array of bacteria and other microorganisms that can be transferred to breast milk during breastfeeding. This transfer of bacteria helps introduce new types of bacteria to the milk, potentially influencing the microbial composition of both mom and baby. It’s essential to note that the transfer of bacteria from the infant’s mouth to breast milk is a normal part of the lactation process and doesn’t necessarily indicate a problem with milk hygiene. In fact, this transfer of bacteria can be beneficial for the infant’s developing microbiome, as it exposes the infant to a diverse array of bacteria that support diversity and commensalism.
Mothers ship microbes from their gut to the breast
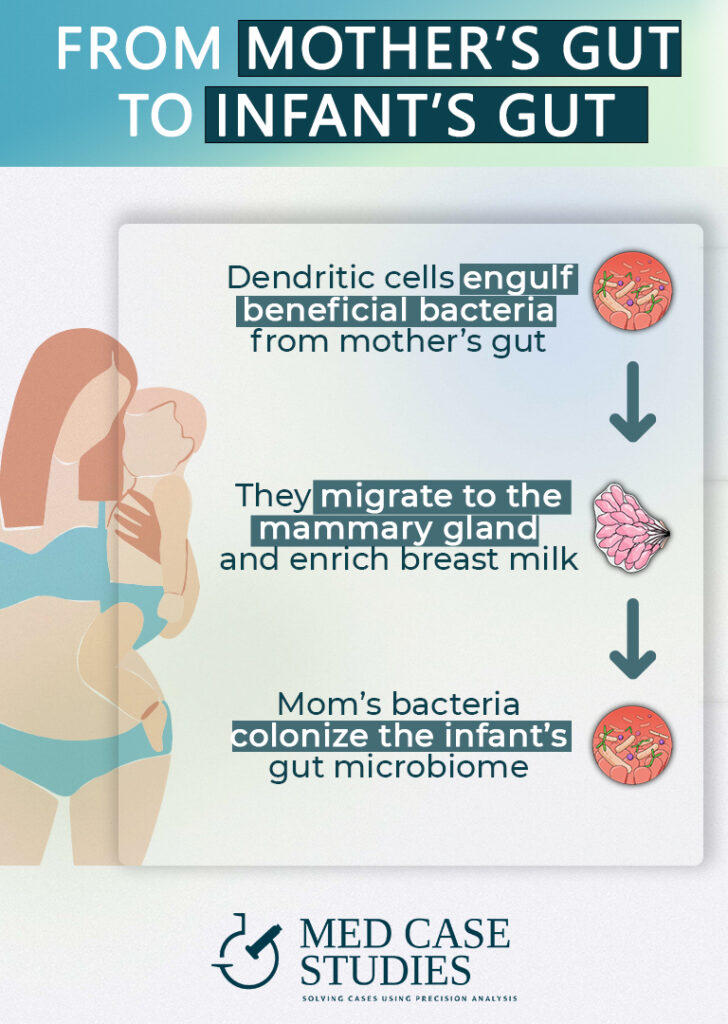
An interesting aspect of the breastfeeding process is that mothers can engulf gut microbes with dendritic cells, enriching the milk and contributing to the diversity of the infant’s gut microbiota composition.
Dendritic cells are immune cells found throughout the body, including the gut. They can engulf and internalize bacteria and other microorganisms through a process called phagocytosis, presenting them to the immune system for further evaluation. This process allows the body to identify and respond to potentially harmful microorganisms.
During lactation, the mother’s gut dendritic cells can engulf bacteria and other microorganisms, transporting them to the mammary gland to be incorporated into the human milk microbiome. This process enriches the milk with a diverse array of bacteria and other microorganisms, contributing to the infant microbiome’s diversity. Overall, breastfeeding involves transferring bacteria and other microorganisms from the mother to the infant, and dendritic cells’ role in enriching the milk with these microbes is a crucial aspect of this process, helping shape the infant’s microbiome composition.
Bacteria in breast milk change composition between feedings
Breast milk is a dynamic and highly nutritious substance that adjusts its composition to meet the evolving needs of the infant, ensuring they receive the right balance of nutrients and beneficial bacteria
Breast milk consists of a complex mixture of nutrients such as proteins, fats, carbohydrates, vitamins, minerals, commensal bacteria, and other microorganisms. It changes over time, particularly in the first few months of life, to meet the baby’s changing needs. For instance, breast milk changes during a feeding: foremilk, produced at the beginning, is thin and watery with more lactose and carbohydrates, while hindmilk, produced later, is thicker and creamier with more fat and nutrients. This change ensures the baby receives a balanced mix of nutrients and energy to support growth and development.
Breast milk also adjusts its composition throughout the day and as the child develops to meet their evolving needs. For example, nighttime breast milk may contain higher levels of certain hormones and substances that promote sleep and relaxation in infants.
Tips for keeping the milk nutritious
Eat a diverse and healthy diet
A healthy and varied diet can help to support the production of milk and may increase the levels of probiotics and prebiotics in breast milk. Aim to include a variety of whole, unprocessed foods in your diet, including fruits, vegetables, whole grains, and lean proteins.
Exercise regularly
Regular physical activity can help to improve overall health and wellness, and it may also have positive effects on breast milk production and quality. Aim to get at least 30 minutes of moderate-intensity exercise per day, such as walking, swimming, or cycling.
Eat prebiotic-rich foods
Prebiotics are non-digestible compounds that serve as potent modifiers of the gut ecology. Including prebiotic-rich foods in your diet, such as onions, garlic, asparagus, and leeks, may help to increase the benefits of breast milk .
Avoid pesticides
Pesticides, such as glyphosate, can be harmful to both human health and the environment. Limiting your exposure to pesticides by choosing organic produce or growing your own, will help reduce the levels of pesticides in breast milk.
Choose healthy fats
Healthy fats, such as olive oil, avocado, and nuts, are an important part of a healthy diet and may support the production and quality of breast milk. Aim to include a variety of healthy fats in your diet to support the production of breast milk.
Take probiotics
Probiotics are beneficial bacteria that can be found in supplements or certain foods. Taking probiotics may help to increase the levels of diversity in the gut, which may be reflected in milk microbiota and optimize infant gut microbiota development.
Avoid processed foods
Processed foods are high in artificial ingredients that should not be present in human milk. Limiting your intake of processed foods and focusing on whole, unprocessed foods will help to improve the quality of human milk bacteria.
Get plenty of sleep
Adequate sleep is important for overall health and wellness, and it may also support the production and quality of breast milk. Aim to get 7-9 hours of sleep per night, choosing most of the days to sleep before midnight.
Stay hydrated
Drinking plenty of water and other fluids can help to support the production of breast milk and may help to improve its quality. besides, milk is mostly composed of just plain water.
Avoid heavy metals
Heavy metals, such as lead and mercury, are harmful to health and are present in certain foods and the environment. Limiting your exposure to heavy metals, such as by avoiding certain types of fish or not smoking, helps reduce the levels of heavy metals in breast milk.
Include seasonal vegetables
Seasonal vegetables are more nutrient-dense than out-of-season produce. They contain a wider range of beneficial nutrients and phytochemicals. Including a variety of seasonal vegetables in your diet helps nourish the microbes in your gut and support milk microbiota.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.