
L-glutamine can cause IBS
learn why and become symptom-free
Diagnosis
Treatment
Follow up
Yes, L-glutamine can cause diarrhea in patients suffering from some forms of IBS. Usually, these patients have increased growth of Proteus mirabilis in their gut, a pathogen that utilizes L-glutamine to exert its pathogenic properties.
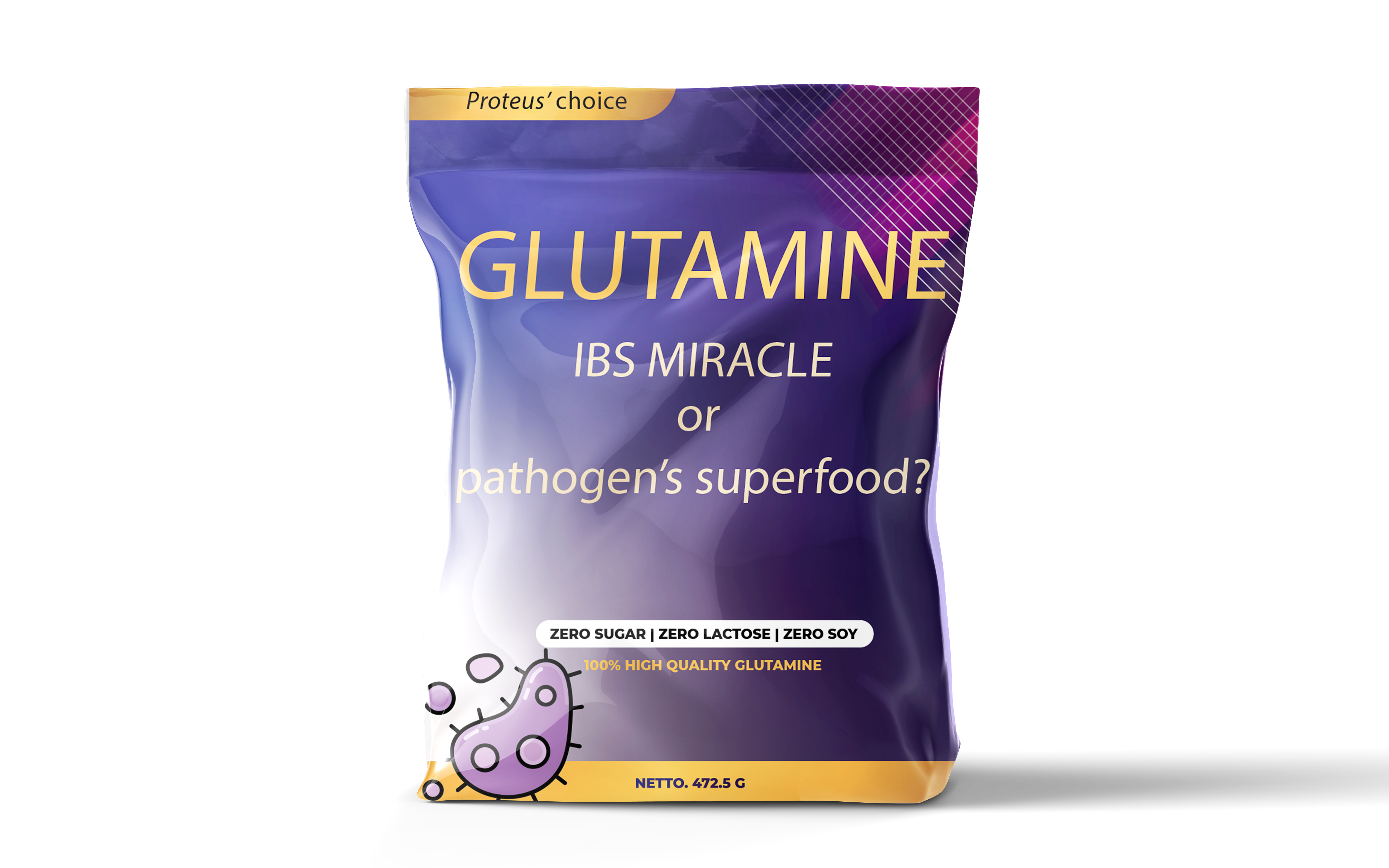
Indeed, glutamine is extremely valuable when it comes to managing functional gastrointestinal symptoms, like bloating and flatulence. Observational and case-control studies have clearly demonstrated the effect of glutamine in restoring intestinal permeability and reducing many troublesome gastrointestinal issues when taken in large amounts. This is why it is widely embraced as a glutamine supplement by both practitioners and patients alike. Moreover, l-glutamine may serve as a vital fuel for intestinal cells, underscoring the need for it to be provided in adequate quantities. Our cells have evolved specific molecular mechanisms to uptake glutamine and transform it into essential products. But are we the only ones capable of harnessing its potential?
Of course, when it comes to the intestinal ecosystem, we are not alone. In fact, we are vastly outnumbered by almost 100 trillion microbes, divided in about 1100 families. Each one of these families has its unique, fingerprint like, metabolism, consisting of hundreds of chemical reactions. Thus, it is not a surprise, that dietary glutamine may be used by other cells (notably bacterial) for their own purposes. In fact, one of the most notorious bacterium, namely Proteus mirabilis, needs excess glutamine quantities in order to exert its pathological properties.

L-glutamine can cause IBS
learn why and become symptom-free
Diagnosis
Treatment
Follow up
First of all it needs glutamine to make protein. That far is ok, since he will use specific amounts of glutamine and that’s all. But what happens when there is excess glutamine in his microenvironment? Proteus possesses another property which is called swarming. This property is defined as the coordinated movement of a population across surfaces. Swarming is initiated under specific circumstances and when there is enough of a specific stimulus. In this case, Proteus will swarm when there is excess glutamine in his environment. Remember that anyone who takes large doses of glutamine will absorb only a minor fraction, and the rest will stay in his gut. Under these conditions, swarming is inevitable. In order for this bacterium to swarm, first it must undergo some morphological and metabolic alterations. In fact Proteus, when in swarming state, acquires antibiotic resistance and produces large amounts of ammonia and other, non gut-friendly products. Actually, in laboratory settings, glutamine is used in order to study the swarming potential of Proteus species.
Proteus has the ability to attach to host tissues with the help of its specialized pili. Once attached, an inflammatory cascade begins that includes molecules with high damage potential, like interleukin-6
Several Proteus species possess the ability to produce large amounts of histamine. This reaction is highly active while Proteus swarms, making it a principle mediator of atopic diseases, like allergies, asthma and diarrhea-predominant IBS
Proteus spc possess strong urease activity. Urease will use extra urea to produce ammonia. In turn, ammonia will make the environment more alkaline and favor the growth of non commensal microbial populations
Proteus species modify their antibitioc resistance gene expression pattern in response to excess glutamine in their environment, making eradication difficult. The longer their populations exist in swarming state, the greatest the antibiotic resistance
Even when Proteus dies, it releases a proinflammatory molecule, namely LPS, which passess through the intestinal barrier and may react with almost every human organ. High LPS levels are detected in people suffering from autoimmune disorders, autism and neurodegenerative diseases like Parkinson’s

L-glutamine gives you diarrhea?
you probably have proteus in stool
Diagnosis
Treatment
Follow up
People who take glutamine may feel better temporarily because it is a trophic agent. It helps restore epithelial junctions and reduce SIBO. The problem begins when there is Proteus (or other swarming bacteria) overgrowth. These patients may feel better for a while, but in fact the problems gets bigger, so the next relapse of their disease may be magnified.
While Proteus is found in almost everyone’s gut ecosystem, it’s concentration is self-regulated as a function of nutrient availability, spatial requirements and host’s immune well being. When these conditions are pathologically altered, Proteus expands. Patients that are susceptible to Proteus overgrowth are:
Most culture techniques report Proteus as negative. Unfortunately, IBS symptoms attributed to Proteus may manifest at these negative levels. Remember that Proteus lives in almost every human gut, so negative just means low levels. Practically, the best way to measure bacterial levels on stool is Mass Spectroscopy. Levels above 10.000 cells per gram of stool may potentially cause symptoms, under several conditions.
Usually, patients with elevated Proteus levels exhibit some form of inflammation. Even individuals diagnosed with IBS, a syndrome traditionally viewed as non-inflammatory often present with raised inflammatory markers, such as CRP or erythrocyte sedimentation rate. Frequently, these patients report abdominal pain that extends beyond their gut, along with stiffness and occasional allergic reactions. It is not uncommon for them to develop autoimmune disorders, whether affecting the bowel or other systems.
Most had more than 1 main complaint
Treatment of IBS patients who are diagnosed with Proteus overgrowth is dependant on the time this bacterium is overgown. Due to its properties, Proteus reconditions its microenvironment and makes it friendly for its own growth. This is why antibiotic treatments may lower bacterial levels, but the remaining favor its regrowth. In fact, eradication in such cases is one of the most difficult tasks, and besides antimicrobial treatment, other treatments and lifestyle changes must be implemented in order to restore gut physiology and reinoculate beneficial microflora.
Every substance, natural or chemical, has its risks when given in therapeutic doses. Glutamine, despite being a naturally occurring amino acid, if taken in large doses may exacerbate several gastrointestinal symptoms. In fact, there is another dark side of glutamine. Many cancers, at certain differentiation stages, use glutamine to survive and spread. Concerning IBS, while glutamine causing worsening of the disease is not very common, it is something I’ve seen many times in my practice. If a patient fulfills one of the above risk factors, a thorough stool test must be performed before scheduling the treatment.
In most cases yes. A clean L- glutamine supplement will help you restore diarrhea-induced gut damage. But, if taking L-glutamine makes you worse in the short- or mid-term, you may have Proteus spp dysbiosis

| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |