
For a step by step walkthrough of tests and treatment, read the dedicated chapter on post-infectious ibs in IBSYNCRASY
-
DIAGNOSIS
TREATMENT
-
FOLLOW UP
Post-infectious IBS treatment should focus on reversing the biochemical and immune changes that the infection left behind and not only aim to calming pain and normalizing bowel habits. Care can be mainstream or personalized, but both work better when the barrier, immune tone, and neural signaling are considered together. Testing that profiles organisms and pathways helps target antimicrobials and microbiome supports while meal spacing and hydration improve engraftment.

and how does it relate to irritable bowel syndrome?
Treatment goals are to reduce gastrointestinal symptom burden, restore healthy bowel habit, and address the drivers left by the infection. Care generally starts with symptom-relieving options, then moves to pathway-matched plans informed by testing. This section covers both.
For people with diarrhea-predominant patterns, rifaximin reduces IBS-D symptoms in high-quality guidance, and short courses can be repeated if benefit wanes. In plain terms, a non-absorbed antibiotic can quiet overgrowth-like patterns without system-wide exposure. Probiotics can help selected ibs patients, but blends should be chosen by target such as gas, stool form, or pain rather than brand. Put simply, match the microbe to the job. Spacing meals protects fasting motility, and evidence shows that MMC occurs during fasting and feeding interrupts it, so many people notice less gas when the MMC runs.
Many do better with targeted diagnostics. PCR stool panels and shotgun metagenomics map organisms, while metatranscriptomics reveals active pathways like bile-acid genes or proteases that amplify symptoms in patients. In short, knowing who is present and what they are doing beats guessing. In pathway-matched care, botanicals or pharmaceuticals are selected for the organisms and mechanisms present, for example some respond to berberine derivatives while others to garlic organosulfurs, and yeast overgrowth requires antifungal planning. Personalization limits trial and error and can speed relief.

DIAGNOSIS
TREATMENT
FOLLOW UP
Mechanisms you can address
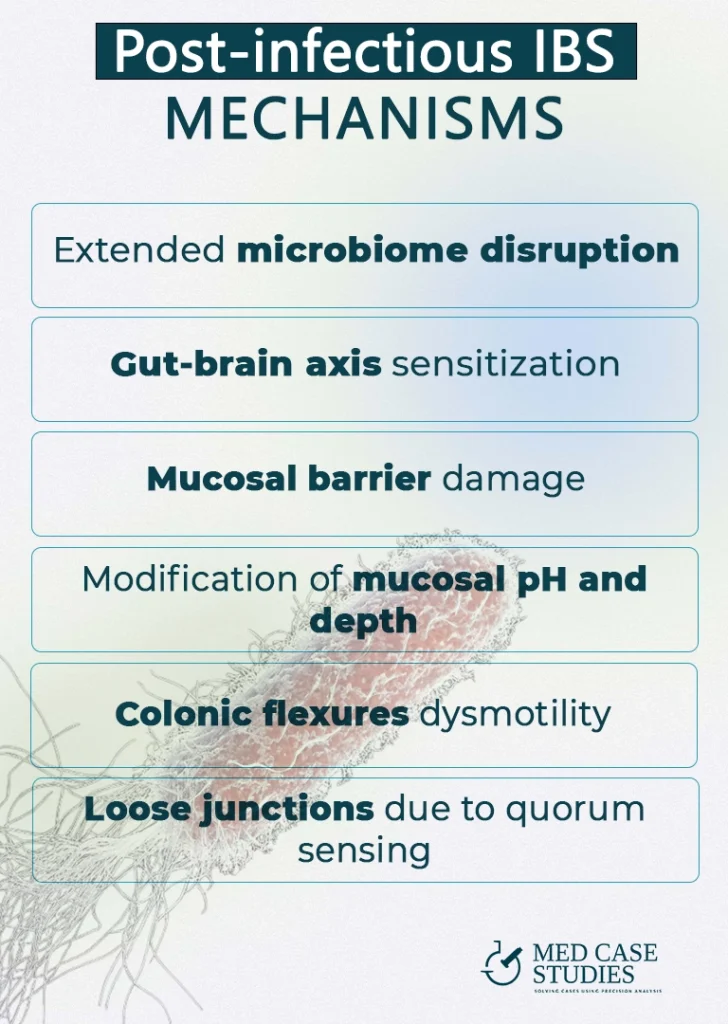
The after-effects of post-infectious illness touch several systems at once. Reviews of postinfectious ibs show that mechanisms include barrier dysfunction, immune activation, and sensory changes that heighten pain signaling. Importantly, there is huge difference between viral and bacterial post infectious development of irritable bowel syndrome. The lining gets leaky, nerves get jumpy, and microbes shift, and together they sustain symptoms. Let’s take a closer look:
An infectious hit can lower commensals and expand fermenters, raising gas and abdominal pain. The mix of bugs changes and produces more irritants. Toxins and enzymes from residual organisms can also stimulate secretion, which worsens stool form in post-infectious ibs.
After infection, colonic afferents become hyperexcitable and amplify normal distension, a hallmark of visceral hypersensitivity in IBS patients. The classic post-infectious neuronal data are shown in the Citrobacter rodentium DRG hyperexcitability paper, which maps well to urgency and pain.
Post-infectious states can thin mucus, alter pH, and reduce secretory IgA, which raises permeability. QS molecules can loosen junctions, and animal studies show that Pseudomonas increases intestinal permeability through interconnected quorum-sensing regulators. What this means for you, supporting the barrier can help many symptoms at once.
Infection-driven motility shifts can leave pockets of gas and stool at the splenic and hepatic flexures, which aggravates bowel habit variability. Traffic lights in the colon get out of sync. Spaced meals and morning activation with light hydration and movement help reset rhythms and reduce symptoms of ibs.
Citrobacter with enterotoxin-driven secretion. Several infectious agent strains of Citrobacter freundii produce a heat stable enterotoxin identical to E. coli STa, which increases chloride secretion and fluid loss and this creates a path to lingering gastrointestinal symptom patterns. Evidence indicates that Citrobacter produces heat-stable toxin, and that secretion load can sustain loose stools.
Pseudomonas aeruginosa with quorum-sensing barrier effects. QS molecules such as 3 oxo C12 HSL modulate tight junctions and can raise permeability, and controlled models show that Pseudomonas increases intestinal permeability via interconnected regulators. Its chatter weakens the fence so irritants slip through.
Proteus mirabilis with mucin and IL 18 axis. Recent work suggests P. mirabilis lowers epithelial IL 18 which reduces mucin, and a thinner mucus layer heightens contact triggered abdominal pain. Supporting mucin and calming inflammation can ease reactivity, and one report shows that Proteus downregulates mucin production in inflamed tissue. Signals like these are also discussed in inflammatory bowel disease even when IBS is the main diagnosis.

DIAGNOSIS
TREATMENT
FOLLOW UP
Treatment works best when it is staged and personalized to your dominant mechanisms. PI-IBS includes diarrhea-predominant, constipation-predominant, and mixed patterns, and each pattern has different levers. Below is the plan I use with patients with IBS who describe an infection-linked onset.
Broad spectrum blends can help, but the best choice comes from testing such as PCR tests or shotgun metagenomics to identify organisms and pathways, then matching strains to gas, stool form, and pain targets
It is common after gastrointestinal infections and is a leading cause of new IBS. Meta analyses suggest a several fold increase compared with uninfected controls.
Most often bacterial infections, though viral and parasitic infections also contribute. Mechanisms include dysbiosis, barrier changes, immune activation, and neural sensitization.
Combine short course rifaximin in IBS D where appropriate, choose goal matched probiotics, protect fasting motility with meal spacing, and consider personalized diagnostics such as PCR, shotgun metagenomics, and metatranscriptomics to target organisms and pathways
Ready for a precision workup? Book a 1:1 consult and we will align PCR, omics, and a targeted antimicrobial–microbiome plan to your gastrointestinal story.
Prefer a step-by-step guide first? My book IBSyncrasy includes a dedicated chapter on post-infectious IBS with exact timelines and dosing frameworks.
Want to read more cases? Start here: post-infectious IBS: viral vs bacterial and this digest on Pseudomonas spp high in stool.

| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |