
learn how your gut works in real life and find your ibs type and treatment in IBSYNCRASY
-
DIAGNOSIS
TREATMENT
-
FOLLOW UP
IBS is a functional bowel disorder, yet people with IBS often have lower baseline micronutrient levels including iron compared with non-IBS controls, which raises the risk of iron deficiency anemia. A systematic review reported lower vitamin B2, vitamin D, calcium, and iron at baseline in IBS cohorts. Anemia itself is not a typical IBS feature and when iron deficiency anemia is present it is a red flag that needs evaluation for other causes like bleeding or malabsorption. The Merck Manual lists iron deficiency anemia among the red flags that warrant investigation.
IBS subtypes behave differently, and knowing your pattern reduces guesswork. If you are not sure where you fit, start with understanding your specific IBS subtype before changing diet or supplements.

DIAGNOSIS
TREATMENT
FOLLOW UP
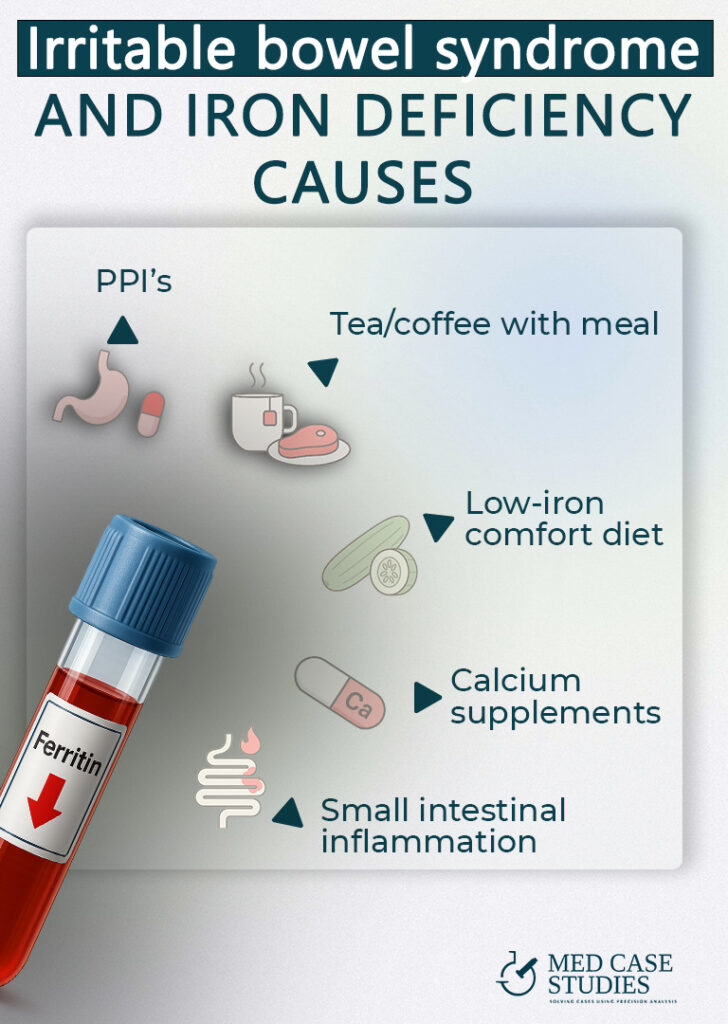
Think of IBS as a risk amplifier. Food avoidance during flares lowers iron intake. Medications and beverages can block non-heme iron absorption. Separate conditions can cause blood loss that reduces iron stores. That is why checking ferritin and iron studies is important, and why stool testing or endoscopic evaluation may be needed if there are alarm features such as rectal bleeding, black stools, or weight loss.
Lower iron intake during strict low FODMAP or when legumes and red meat are reduced
Coffee and tea polyphenols phytates in grains and legumes and calcium at the same meal
Proton pump inhibitors reduce non heme iron absorption even when intake is adequate
Pair iron rich foods with vitamin C and keep coffee tea and calcium away from that meal
Day-to-day choices matter. A low FODMAP phase or other restriction can reduce overall micronutrient intake, including iron, if it is not guided and re-expanded. In a randomized program, the low FODMAP arm had a significant decrease in several micronutrients compared with a standard IBS diet, indicating a real risk if the diet is not supervised.
During the strict low FODMAP phase, people often drop legumes and some grains that carry non-heme iron. If meats are also limited due to symptoms, total iron intake can fall. Data on micronutrient shortfalls during low FODMAP phases come from Eswaran 2020.
Proton pump inhibitors reduce gastric acidity and suppress the absorption of dietary non-heme iron. This has been shown even when intake is adequate. Tea and coffee are potent inhibitors of non-heme iron absorption in humans, which is why beverage timing matters for people with IBS who already struggle with intake. Calcium blocks both heme and non-heme uptake at the enterocyte, so avoid pairing high-calcium foods or supplements with your iron-rich meal. StatPearls. For PPI-focused cases, see my case study on long-term PPI use complicating IBS.
Oral iron commonly causes abdominal pain, bloat, stool darkening, and diarrhea or constipation. Beyond symptoms, luminal iron can shift the gut microbiome toward potentially pro-inflammatory patterns in some settings. A review summarizes that oral iron may adversely affect the intestinal microbiota.
In adults, ferrous bisglycinate increased the relative abundance of Enterobacteriaceae in a controlled study, which aligns with reports that excess luminal iron can favor pathobionts. Clinically, that shift means more gas, urgency, or loose stool for people with IBS who are already sensitive to microbial and metabolic changes.
Many people with IBS report that standard oral iron worsens diarrhea, bloat, or abdominal pain. If an oral trial is essential, using the lowest effective dose, alternate-day dosing, or slow-release formulations can sometimes improve tolerance, yet symptoms can still persist. After antibiotics, animal data suggest oral iron may hinder microbiota recovery, which is another reason to be cautious soon after antibiotic courses. In our practice we see this pattern often, especially in people with post-infectious IBS or recent antibiotic exposure.

DIAGNOSIS
TREATMENT
FOLLOW UP
Because IBS is a microbiome-sensitive condition, our GI-microbiome–first stance is to avoid oral iron whenever possible, to protect the gut environment and symptoms. We prefer medically supervised intravenous iron when iron repletion is necessary, since it bypasses the intestinal lumen and is effective without exposing the gut to unabsorbed iron. Best-practice advice supports IV iron when oral iron is not tolerated, ineffective, or absorption is compromised. See the AGA 2024 Clinical Practice Update. We reserve liposomal oral iron for very extreme situations where IV is not feasible and a short, closely monitored course is the only practical option.
IV iron achieves repletion quickly without leaving free iron in the intestinal lumen, which reduces the chance of feeding Enterobacteriaceae or aggravating IBS symptoms. It avoids beverage and calcium interactions, and it is not limited by PPI therapy. In our experience with people who have IBS and low iron, symptom stability is often better when IV iron is used under supervision compared with repeated oral trials.
I recommend liposomal iron only in rare scenarios when a carefully monitored, short oral course is unavoidable. Even then, we space it away from tea, coffee, and calcium, pair with vitamin C, and stop if abdominal pain, diarrhea, or bloat escalate. If intolerance appears, we stop and route to IV iron rather than forcing adaptation.
Choose heme iron sources you tolerate and pair non-heme iron with vitamin C. Re-expand a low FODMAP diet to include iron-containing foods as soon as your symptoms allow. If SIBO or another condition is suspected, address it because overlapping issues can lower iron or vitamin B12. Learn why diagnosing the specific bacterium in SIBO can influence iron and B12 status.
Heme iron from meats is absorbed more efficiently and is less affected by inhibitors. Non-heme iron from legumes, fortified grains, nuts, and leafy greens benefits from vitamin C pairing. Keep a weekly rotation that fits your IBS subtype and symptoms, and avoid combining your iron-rich meal with tea, coffee, or calcium.
Common GI causes include inflammatory bowel disease, celiac disease, peptic ulcer disease, colorectal cancer, angiodysplasia, and other sources of occult bleeding. Guidelines recommend evaluating iron deficiency anemia for gastrointestinal sources rather than assuming IBS alone.
Yes. Systematic reviews describe lower baseline iron among IBS cohorts and clinical studies show that anemia in suspected IBS predicts organic disease rather than IBS itself. Major societies advise a structured GI evaluation when iron deficiency anemia is present. See the multicenter alarm-feature study and the IBS micronutrient review.
Map your IBS subtype, correct the cause of low iron, and pick the least disruptive repletion path. If you want the full playbook built from over a thousand real cases, get the book IBSyncrasy and start personalizing your plan today. Buy the book.

| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |