SIBO after gallbladder removal
SIBO after gallbladder removal occurs in more than 80% of all cases, from 6 months to 7 years post-surgery. And this is only from my experience. Even if your symptoms existed before the operation, digestive issues like bloating, abdominal pain, and irregular bowel habits, continue to exist or even get intensified
💬 Gallbladder removal alters the duodenal pH favoring the overgrowth of bacteria. Use the live chat in the bottom-right to ask me anything in real time.
Article Highlights
SIBO is defined as an increase in the number of bacteria (103–105 CFU/mL), an alteration in the bacterial composition, or both in the small intestine.
SIBO after cholecystectomy is a physiological consequence of the digestive diversion
Over 80% of my cases develop SIBO within 7 years from cholecystectomy
Restoring normal small intestinal growth is doable but several lifestyle and dietary interventions should become permanent
Dividing fat content per meal, proper posture during eating, early dinner and several herbal teas are unexpected but very important parts of healing

Table of Contents
Many patients, especially women who have experienced childbirth find that their symptoms persist or even worsen after gallbladder removal. As a microbiome researcher and practitioner with over 4,000 cases under my belt, I’ve seen firsthand how gallbladder removal surgery can trigger small intestinal bacterial overgrowth (SIBO) and change the very nature of your digestion.
Gallbladder function and digestion 101
First of all, your gallbladder is not just a bile-storing bag. It is a remarkable organ that has evolved over millennia to play a crucial role in fat digestion, fat-soluble detoxification and also glandular excretions. It stores and concentrates bile, a digestive fluid produced by the liver that is rich in bile acids. Bile not only aids fat digestion but also helps maintain a healthy bacterial balance in your small intestine.
No matter the gallbladder disease that led to the surgery (gallstones, polyps or cholecystitis), when you undergo cholecystectomy the controlled flow of bile is replaced by a constant bile flow into your intestinal tract. So now you have bile 24/7 but always less than needed. This shift affects the bile acid pool and the natural balance of bacterial populations, setting the stage for issues like malabsorption and SIBO.
How gallbladder removal contributes to SIBO (and IBS)
After the gallbladder is removed, the deficiency of SP-D, a substance normally produced by the gallbladder that supports bacterial balance can have significant effects on your digestive system. This protein makes sure that the majority of your intestinal bacteria stay where they are supposed to stay. That is you large intestine. But, the loss of this regulatory factor means that the flow of bile becomes constant rather than episodic, altering the pH of the small intestine.
This constant bile environment may not be as effective at controlling bacterial populations, allowing bacterial overgrowth to flourish. In fact, the diagnosis of SIBO is very common after gallbladder removal, with clinical observations showing that more than 80% of my patients experience symptoms related to SIBO.
When SIBO develops, it’s not just methane-induced overgrowth you’re dealing with. Hydrogen production and other bacterial by-products can also contribute to symptoms like bloat, abdominal pain, and changes in stool consistency. A hydrogen breath test is often used to diagnose SIBO, measuring levels of hydrogen and methane in your breath, but in my experience it provides limited therapeutic value
Symptoms beyond digestive issues
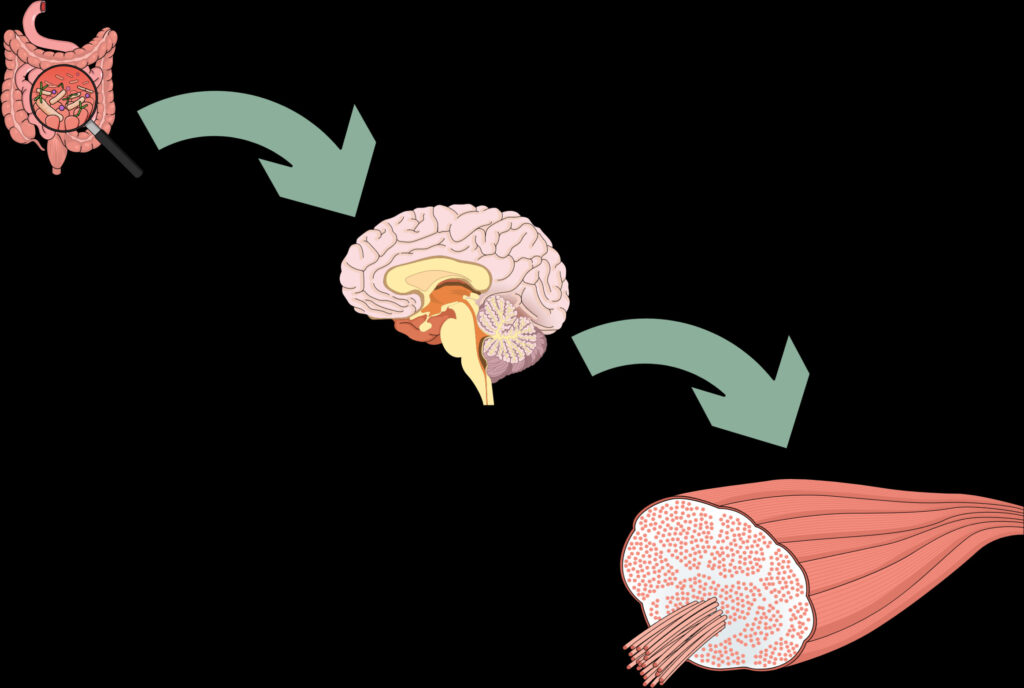
Irritable bowel syndrome symptoms are not the only result from the removal of your gallbladder. It can set off a cascade of symptoms that extend well beyond your gut. Without your gallbladder to regulate the flow of bile and support the production of SP-D, your digestive system loses an important control mechanism. And it is well-known that your gut is critical regulator of all other organs in our body
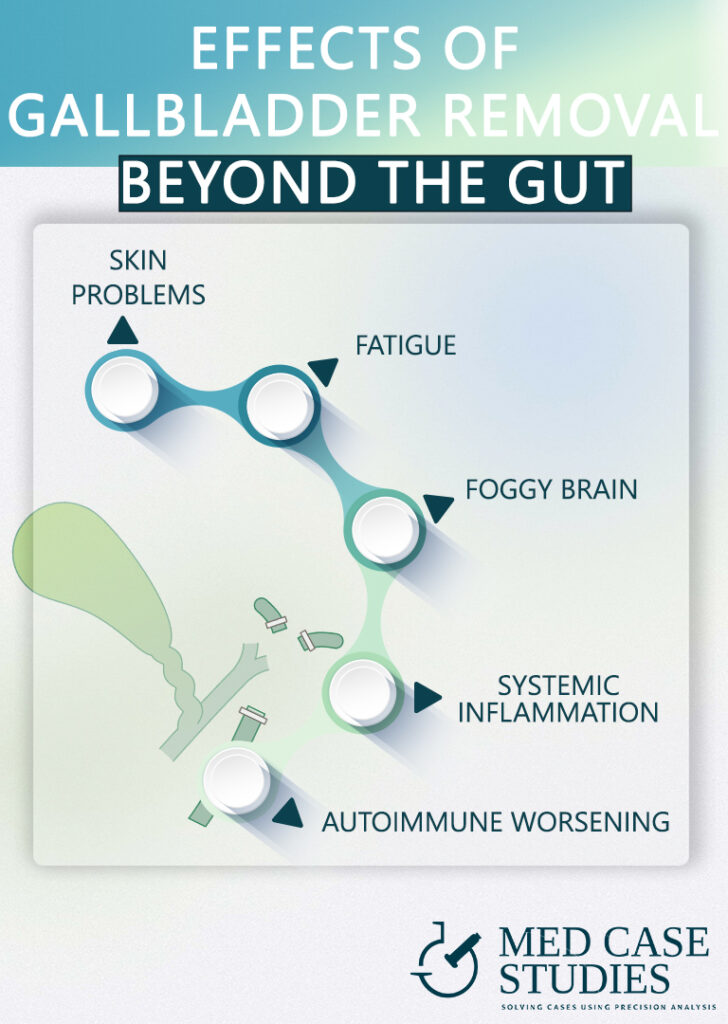
Skin diseases
One of the most noticeable extraintestinal manifestations is the development of skin disorders. Patients often report outbreaks of acne and eczema following gallbladder removal. Acne may emerge as bacterial overgrowth leads to systemic inflammation, while eczema can be aggravated by an imbalanced immune response that no longer benefits from the gallbladder’s regulatory effects. These skin conditions are visible signs that the changes in your digestive system are influencing your overall health.
Fatigue and fibromyalgia
Beyond skin issues, the inflammatory state induced by SIBO in patients frequently contributes to a deep-seated fatigue, an exhaustion that isn’t resolved by rest and can severely impact daily activities and quality of life.
Foggy brain and joint pain
In addition to skin disorders and fatigue, many patients experience cognitive and musculoskeletal challenges. A common complaint is brain fog, characterized by difficulties in concentration and memory lapses that disrupt both professional and personal routines. Another extraintestinal symptom often reported is joint pain, which can stem from chronic inflammation and the systemic stress caused by the altered bile flow. These symptoms underscore that the effects of gallbladder surgery and SIBO are not confined to the digestive tract but reflect a broader disturbance in your body’s natural physiology.
Initial actionable steps to manage SIBO
The good news is that the changes in your digestive system after gallbladder removal can be managed with actionable steps. First, dietary modifications can make a huge difference. The timing of your last meal, the percentage of fat per meal, the beverages and teas you are consuming even the posture you have when you are eating are very important to counteract the loss of this organ. Of course, regular physical activity and stress management also improve intestinal motility but may help stabilize your bacterial balance. In my extensive clinical experience, patients who commit to small, consistent lifestyle changes see significant improvements in their symptoms.
- Include a lower dose of healthy fat with every meal. Aim for about 5 to 7 grams. This might mean adding exactly one teaspoon of extra virgin olive oil to your salad, incorporating a quarter of an avocado into your bowl, or having 10–12 raw almonds as a snack. The goal is to stimulate bile release without overwhelming your digestive system
- Wait about 20–30 minutes after a meal before drinking significant amounts of water. This practice prevents the dilution of bile and digestive enzymes, allowing them to work more effectively on the fats present in your food.
- Consider ox bile extract before heavy meals. This may help mimic the concentrated bile you once had. This supplement is designed to boost the emulsification process, improving fat digestion and nutrient absorption
- Pre-meal acidification. The increased gastric acidity promotes better emulsification of dietary fats and facilitates more efficient digestion. This targeted intervention not only aids in fat breakdown but also helps suppress the growth of unwanted bacteria in your small intestine, reducing the risk of small intestinal bacterial overgrowth.
- Chew your food slowly and thoroughly. This extra effort mechanically breaks down food particles, allowing digestive enzymes and the less concentrated bile to work more effectively.
Are probiotics good after gallbladder removal?
The answer is yes, but only once you’ve created conditions that favor their effectiveness. Constant alkalinization of your small intestine may work against the benefits of probiotics. Therefore, the first step is to modify your diet and lifestyle to restore a more balanced bile acid environment. Once your digestive system begins to normalize, carefully selected probiotics can further support your bacterial balance and help address SIBO.
Personalized treatment and ongoing management
After your gallbladder is removed, a personalized treatment and lifestyle plan becomes essential. The loss of this vital organ alters your bile flow and digestive physiology, leading to challenges that extend beyond typical gut discomfort. While SIBO can be eradicated through targeted therapies, if you don’t maintain the recommended dietary and lifestyle changes, the condition is likely to reoccur. This is because the delicate balance in your intestinal bacterial ecosystem is continuously disrupted, paving the way for intestinal bacterial overgrowth in patients.
Globally, millions of cholecystectomies are performed each year, a statistic that underscores the widespread impact of this surgery. Studies have shown that the prevalence of SIBO in patients with a gallbladder removed is significantly higher compared to individuals with an intact gallbladder. The increased incidence of intestinal bacterial overgrowth in patients highlights the importance of recognizing that SIBO is not just a transient issue but a recurring challenge that requires ongoing management.
Ultimately, successful management of SIBO after cholecystectomy hinges on a continuous, multifaceted approach. And this is something I came across daily in my practice. This involves not only eradicating the overgrowth through appropriate treatments but also sustaining a regimen that supports a balanced digestive system. Remember, the benefits of treatment can be short-lived if recommendations are not followed consistently.
FAQ: SIBO after gallbladder removal
How common is SIBO after gallbladder removal?
From my clinical experience, more than 80% of cases develop SIBO within seven years after cholecystectomy. Research also shows higher prevalence in cholecystectomy patients than in people with an intact gallbladder.
Why does gallbladder removal contribute to SIBO?
After surgery, bile flows constantly and is less concentrated, altering small-intestinal pH. The loss of supportive factors (like SP-D) weakens bacterial control, allowing overgrowth.
SIBO symptoms beyond digestion?
Skin issues (acne/eczema), fatigue or fibromyalgia-like pain, brain fog and joint pain can appear alongside bloating and abdominal discomfort.
Are probiotics good after gallbladder removal?
Yes—once the environment is favorable. First adjust diet and meal timing to restore a healthier bile-acid balance; then add targeted probiotics.
What initial steps help manage SIBO?
Include ~5–7 g healthy fat per meal, wait 20–30 minutes before drinking water, consider ox bile before heavy meals, use pre-meal acidification, and chew slowly and thoroughly.
Do I need a breath test?
Hydrogen breath tests are commonly used, but in my experience they have limited therapeutic value. Treatment and sustained habits matter most.

Theodoros Prevedoros, MSc
The Microbiome Biochemist
With extensive experience evaluating over 3000 cases in various specialties, including gastroenterology, pediatrics, and endocrinology, Theodoros has collaborated with more than 25 doctors from Greece and Cyprus and over 10 laboratories worldwide.
With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.
With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.
More posts