High-salt diets and hypertension: A gut microbiome point of view
Unearthed: ancient Roman soldiers earned their "salary" in salt, a vital mineral for health, making this "white gold" a priceless treasure in history!
Once upon a time, salt (sodium chloride) was a precious commodity, so valuable it was sometimes referred to as “white gold.” Its use dates back to ancient civilizations, where it played a crucial role in both preserving food and enhancing its flavor.
Historical use of salt: preservation and flavor
Preservation and taste
Before the age of refrigeration, salt was the go-to method for preserving food, as its antimicrobial properties helped keep the bad bacteria at bay. It worked by drawing moisture out of the food, creating an inhospitable environment for any microbial party-crashers. This was particularly important for preserving meat and fish, ensuring that food could be stored for extended periods without spoiling. For example, ancient Egyptians used salt to preserve their fish and meat, which was essential for the survival of their civilization, especially during lean times.
But salt wasn’t just about preservation; it was also about taste. The ancient Romans loved their salty fish sauce called “garum,” a funky concoction of fermented fish guts and salt, which they splashed on pretty much everything (yum!). The Aztecs were also known to add a pinch of salt to their cocoa drinks, intensifying the flavor and making it a divine treat.
Salty revolution
Perhaps the most famous salt-related historical event is the infamous “Salt March” led by Mahatma Gandhi in 1930. This 240-mile trek protested the British monopoly on salt production and sales in India, which resulted in high salt taxes and restricted access to this vital resource for the Indian population. The march led to civil disobedience and ultimately played a role in India’s fight for independence.
Despite its significant historical role, we now know that too much salt in our diets can lead to health problems like hypertension, cardiovascular disease, and kidney disease. So while we still appreciate its ancient uses in preservation and flavor, we also recognize the importance of keeping our salt consumption in check.
Global salt consumption: The current scenario
As we continue our savory journey, let’s take a look at the present-day global salt consumption landscape. It’s no secret that we humans love our salt, but the extent of our sodium infatuation varies across countries and cultures.
In general, most people consume more salt than recommended by health authorities. The World Health Organization (WHO) advises a daily sodium intake of less than 2,000 milligrams (equivalent to 5 grams of salt) for adults. However, the average person consumes about 9-12 grams per day. That’s a lot of extra salt on our plates!
One reason for this disparity is the influence of globalization and the food industry. As the world becomes more interconnected, we’ve seen a rise in the popularity of processed and fast foods, which often contain high levels of sodium. These sneaky sodium bombs can make it challenging to maintain a low-salt diet, even for those with the best intentions.
Cultural differences also play a role in salt consumption. For instance, Japan is known for its love of soy sauce and salty broths, leading to a higher average salt intake compared to other countries. On the other hand, the Mediterranean diet, praised for its heart-healthy benefits, emphasizes fresh fruits, vegetables, and lean proteins, which generally contain lower amounts of sodium.
How does a high-salt diet affect our health?
Let’s take a closer look at the impact of high-salt diets on various human systems, the related disorders, and their symptoms.
Human System Affected | Disorder | Symptoms |
|---|---|---|
Cardiovascular | Hypertension (High Blood Pressure) | Headaches, dizziness, blurred vision, shortness of breath, nosebleeds |
Cardiovascular | Cardiovascular Disease | Chest pain, shortness of breath, pain in arms or shoulders, nausea, lightheadedness |
Renal (Kidney) | Kidney Disease | Swelling in hands and feet, fatigue, changes in urine output, skin rash, metallic taste in mouth |
Immune System | Autoimmune Disease (e.g., Multiple Sclerosis) | Varies by disease, but may include muscle weakness, fatigue, numbness, tingling, or pain |
Gastrointestinal | IBS | Bloating, gas, abdominal pain, diarrhea, constipation, changes in appetite |
Neurological | Stroke | Sudden numbness or weakness, confusion, trouble speaking, severe headache, dizziness |
As the table illustrates, excess sodium intake can wreak havoc on various systems in our bodies, from our heart and blood vessels to our kidneys and gut microbiome. High sodium intake can lead to hypertension, which is a significant risk factor for heart disease, stroke, and kidney problems. Additionally, an imbalance in our gut bacteria, known as dysbiosis, can occur due to high salt consumption, leading to gastrointestinal issues and even contributing to autoimmune diseases
Enter the gut microbiome: The connection to high-salt diets
Our gut is home to trillions of bacteria that play a crucial role in our overall health, from digestion to immunity. Recent research has shed light on how high-salt diets can affect the composition of these gut microbes, leading to imbalances and health issues.
In a study focused on animal models, a diet high in sodium was found to alter gut microbiota composition and the levels of microbial proteins in the gut. This change in the gut’s microbial profile was characterized by a loss in diversity and a shift in composition. The study observed that mice on a high-sodium diet had higher levels of Firmicutes but lower levels of Bacteroidetes compared to those on a low-salt diet. This increase in the Firmicutes/Bacteroidetes ratio has been associated with cardiovascular diseases and obesity in previous research.
Furthermore, the high-sodium diet group had higher abundances of Lachnospiraceae and Ruminococcus but lower abundance of Lactobacillus compared to the low-salt diet group. This is particularly interesting, as Lactobacillus is a beneficial probiotic bacterium known to support gut health.
The mechanism of salt-induced dysbiosis
The study also explored the potential mechanisms behind these changes in gut microbiota. Sodium chloride absorption in the gut is mediated by a process of bulk flow along an osmotic pressure gradient. Na+/H+ exchange, a membrane transport mechanism, is involved in intestinal sodium chloride transport and regulating the gut microbial environment. High sodium intake increases the activity of apical Na+/H+ exchange, which is closely correlated with gut microbiota composition.
The researchers suggested that the high-salt diet may increase Na+/H+ exchange activity, which in turn alters the gut microbial profiles. It’s important to note that high sodium intake doesn’t cause total body water storage but induces a fluid shift from the interstitial to the intravascular space. This fluid shift may affect the excretion of digestive enzymes in the small intestine, which could further influence gut microbiota composition.
Microbiome-Kidney axis: A key player in hypertension prevention
Now, let’s turn our attention to the microbiome-kidney axis. The kidneys play a significant role in blood pressure regulation, making this interaction particularly important when examining the effects of high-salt diets on our health.
One key component in the microbiome-kidney axis is acetate, a gut metabolite produced by certain beneficial bacteria when they break down dietary fiber. Acetate has been shown to play a role in blood pressure regulation, making it an essential factor in the relationship between gut health and kidney function.
When we consume a high-salt diet, the changes in gut microbiota can lead to imbalances in the production of SCFAs, including acetate. This imbalance can disrupt the delicate microbiome-kidney axis, affecting kidney function and blood pressure regulation. As a result, high-sodium diets can contribute to hypertension and other cardiovascular diseases.
Reducing salt intake: How can we make our bacteria happy?
Mind your seasonings: Instead of relying on salt to flavor your food, experiment with herbs, spices, and other natural flavor-enhancers like lemon juice or vinegar. This will not only reduce your salt intake but also introduce new, exciting tastes to your meals.
Embrace whole foods: Processed and packaged foods often contain high levels of sodium. Opt for fresh fruits, vegetables, whole grains, and lean proteins to keep your salt intake in check.
Read labels: When shopping, pay attention to the sodium content on nutrition labels. Look for low-sodium or no-salt-added options, and be cautious of sneaky sources of sodium, like canned soups or sauces.
Go Mediterranean: Sticking to a Mediterranean-based diet has been shown to improve hypertension, partly through the optimization of the gut microbiome
Cook at home: Preparing your meals allows you to control the amount of dietary salt you use. Experiment with salt-free recipes, and remember that a little goes a long way.
Stay hydrated: The gut-kidney axis is crucial for regulating hydration in the body, and excess salt intake is disrupting this axis making the water molecules less available.
My experience
As a biochemist specializing in gut health, I’ve seen remarkable transformations in my patients’ overall well-being. One striking observation is how their blood pressure tends to normalize when we address gut-related issues. This fascinating connection between the gut and kidney highlights the incredible impact that lifestyle, dietary, and behavioral adjustments can have on our health. By simply modifying one’s diet to alter the gut microbiome, we can potentially change the course of hypertension at its very onset. The interplay between changes in the gut and a salt-heavy diet is particularly noteworthy, as reducing sodium intake can be a powerful tool in managing this silent yet dangerous condition. It’s astonishing to see how a healthier gut can lead to such a profound ripple effect on our bodies, proving that taking care of our inner ecosystem is truly essential for overall well-being.
Send an email for further information or to discuss how I can help you achieve your health goals by addressing your gut health and microbiome. Book an appointment to receive personalized guidance and support, tailored to your specific needs.

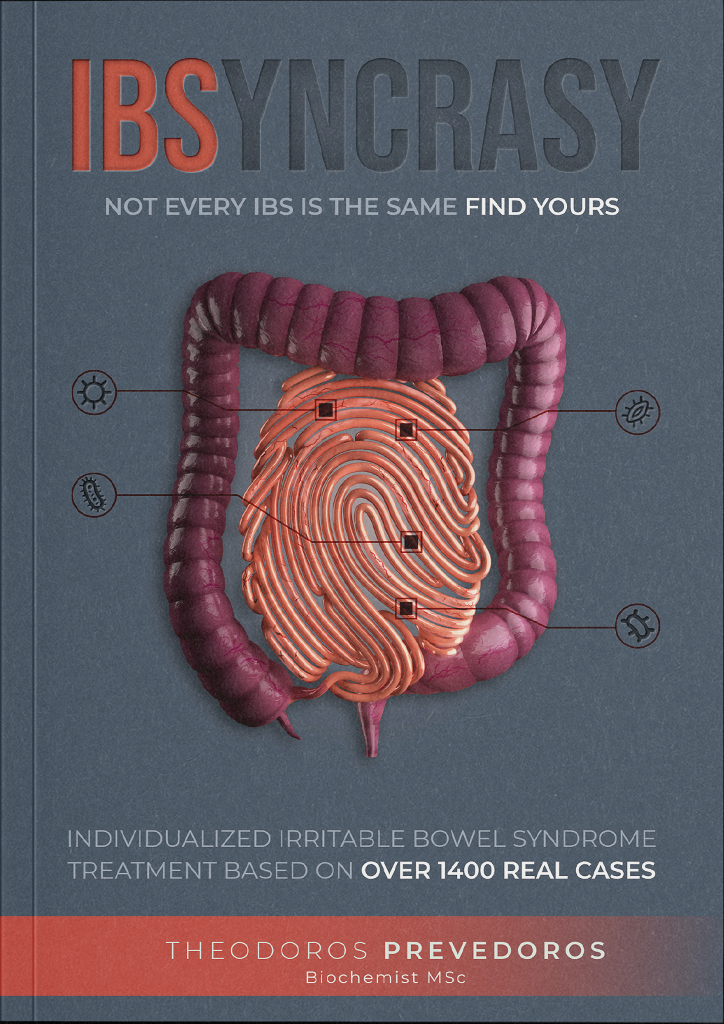
With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.