SIBO Success Stories: It feels like IBS

Number of cases
Mean age
Rate of success
Treatment duration
Most common symptom
Most common culprit
symptoms
Microbes, neurons and the gut
The small intestine, vital for digestion, can suffer from small intestinal bacterial overgrowth (SIBO), disrupting motility and causing IBS. Our intestinal system has energy-consuming phases, like eating, and anabolic repairing phases controlled by hormones and the central nervous system. Inflammation and immune activation result from digestion, bacteria, and toxins. It’s crucial to give our intestines time to repair and resolve inflammation.
The role of migration motor complex (MMC)
MMC, a neurological process, is responsible for cleaning the small intestine. It helps to move food and waste through our body. It happens when we are not eating, like during sleep or between meals. If the MMC cannot perform its tasks, IBS is inevitable. Addressing the root cause of SIBO and implementing proper treatment, such as antibiotics or antimicrobials, is crucial for gut health.
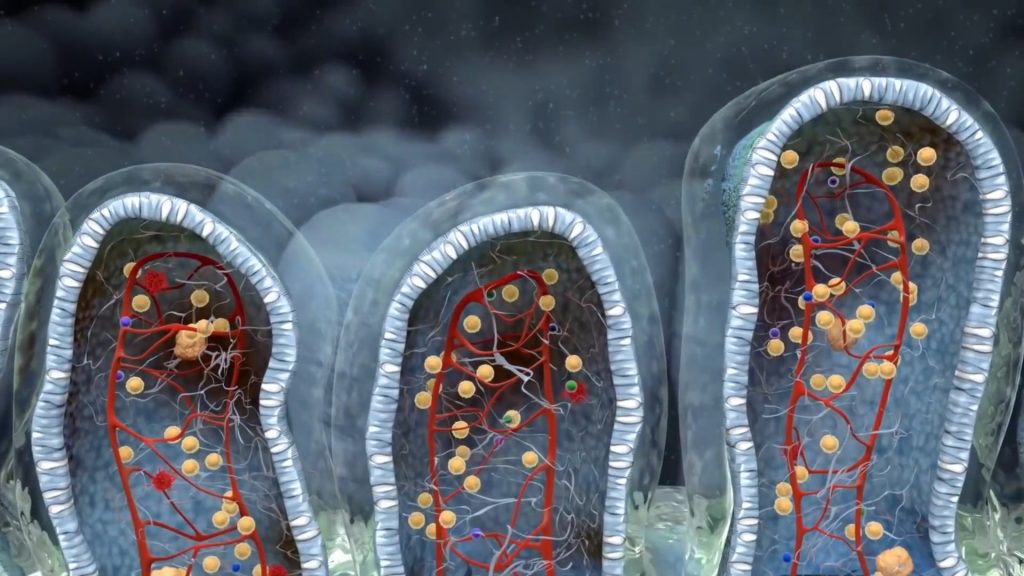
The waves of MMC, or Migrating Motor Complex, are movements that happen in our digestive system. They are divided into four phases:
Phase I: This is the resting phase. There is very little movement in the stomach and intestines during this time.
Phase II: This phase has irregular contractions. The movement starts to increase slowly, preparing the digestive system for stronger action.
Phase III: This is the active phase. Strong and regular contractions happen in the stomach and intestines, helping to push leftover food and waste forward.
Phase IV: This phase is a transition between the active and resting phases. The contractions start to slow down and become less regular.
These waves repeat every 90-120 minutes when we are not eating, helping to keep our digestive system clean and healthy.
Colin, a popular 24-year-old postgraduate student, had an active social life with late nights and occasional alcohol consumption. Diagnosed with Hashimoto’s hypothyroidism, he started experiencing gut health issues like burping after meals, bloating, and acute abdominal pain. Despite numerous gastroenterologist visits, gallbladder removal, and even antidepressant prescriptions, his SIBO symptoms remained unresolved.
Thyroid diseases, either hypo- or hyper- thyroidism affect the vagal regulation of small intestinal contractions
Persistent histamine release can alter gastric and small intestinal contractions, contributing to digestive issues and potentially SIBO symptoms.
Eating every three hours may hinder the cleaning mechanism (MMC) from performing its necessary repairing activities, causing SIBO and impacting gut microbiome health.
Bile acids are essential regulators of Phase III MMC. Gallbladder removal results in different bile acid pools, potentially compromising proper intestinal motility and increasing the risk of small intestine bacterial overgrowth.

Colin firmly believed that his lifelong eating habits, with breakfast right after waking up and the last meal always after 10 pm, shouldn’t be causing his gastrointestinal symptoms. He thought he maintained a “good” meal schedule.
The thyroid gland plays a crucial role in regulating the gut-brain axis, including the Migrating Motor Complex (MMC). Any deviation from normal thyroid function can significantly impact both neural control of gut movements and hormonal regulation of GI secretion.
Although allergies are classically associated with antibody production, there is often an excess of histamine in allergy-prone patients. Antihistamines are frequently effective because of this. However, histamine also plays a role in partly inhibiting neurogastromotility, such as the vagal regulation of MMC.
Gallbladder removal may not have been the root cause of Colin’s symptoms, as it was performed later, but it certainly worsened both their intensity and duration. Studies have shown that gallbladder removal slows down the Migrating Motor Complex and is statistically linked to a higher incidence of (SIBO).
While disorganized MMC was only a hypothesis at that point, many of Colin’s symptoms pointed in this direction. The timing of his burping, gas, and bloating in accordance with his eating patterns (even then, five meals every three hours) seemed to form a plausible diagnosis for SIBO.
Digestive residues
Fragments and residues of undigested food particles cause mixed movements in the gut, leading to an alternating defecation pattern.
Elevated stool EPX/histamine
Both of these substances mediate allergic reactions in the intestine and other organs.
SIBO
When bacteria are overgrown in the wrong location (small intestine) they may interfere with proper absorption of nutrients and may produce gas and bloating
Probiotic sterility
Probiotic sterility leads to abnormal fermentation of starch, sugars and fiber. Bloating and gas are main symptoms
Treatment for cases like Colin’s should address the entire gastrointestinal system, including the gastric phase, microbial overgrowth in the duodenum and jejunum, and colon microbiome. Although this can be a challenging and time-consuming process, Colin was determined to improve his condition as a 26-year-old. The treatment provided simultaneous antimicrobial activity for both the small and large bowel. The specific treatment varies depending on factors such as the time since gallbladder removal, the extent of SIBO, and the patient’s age. The golden rule is that the earlier the intervention, the better the results. An elemental diet or choosing low FODMAP foods are very useful approaches but should be cautiously implemented and for no more than 3 months. Additionally, in my experience abstaining from gluten is very useful, as the duodenal villi are already very vulnerable due to SIBO.

In a follow-up phone call, Colin mentioned significant improvement in his stool pattern, but also an increase in allergic symptoms. I explained that this was normal and even desirable, as histamine-producing bacteria release large quantities of histamine as they die off. I reassured him that his allergies would likely improve after completing both antimicrobial treatments. He had managed to adjust his meal schedule, but I encouraged him to eat dinner even earlier.
The Migrating Motor Complex (MMC) is the link between the brainstem and the gut, acting as the neurological control panel for gastric contractions between meals and during fasting. As these contractions are propagated by the vagus nerve, the MMC is an essential mechanism for efficient cleansing after digestion, often called the “bowel’s housekeeper.” Fasting during waking hours is crucial, as MMC is naturally downregulated during sleep. Regardless if an IBS-SIBO patient suffers from diarrhea or constipation, fasting during treatment often leads to better results.
- Habits and substances that inhibit Migration Motor Complex will always favor small intestinal bacterial overgrowth
- Allergies should be considered as a potential MMC inhibitor when assessing IBS cases
- Post-meal symptoms, bloating, and stress-induced symptoms are common complaints among IBS patients diagnosed with SIBO
- The vagus nerve plays an important role in how patients experience and report their digestive symptoms, highlighting that IBS is a systemic disorder.
- Lifestyle choices play a crucial role in achieving complete remission, with early treatment leading to better prognosis

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.