IBS or Intestinal Disaccharidase Deficiency? Find out on your own
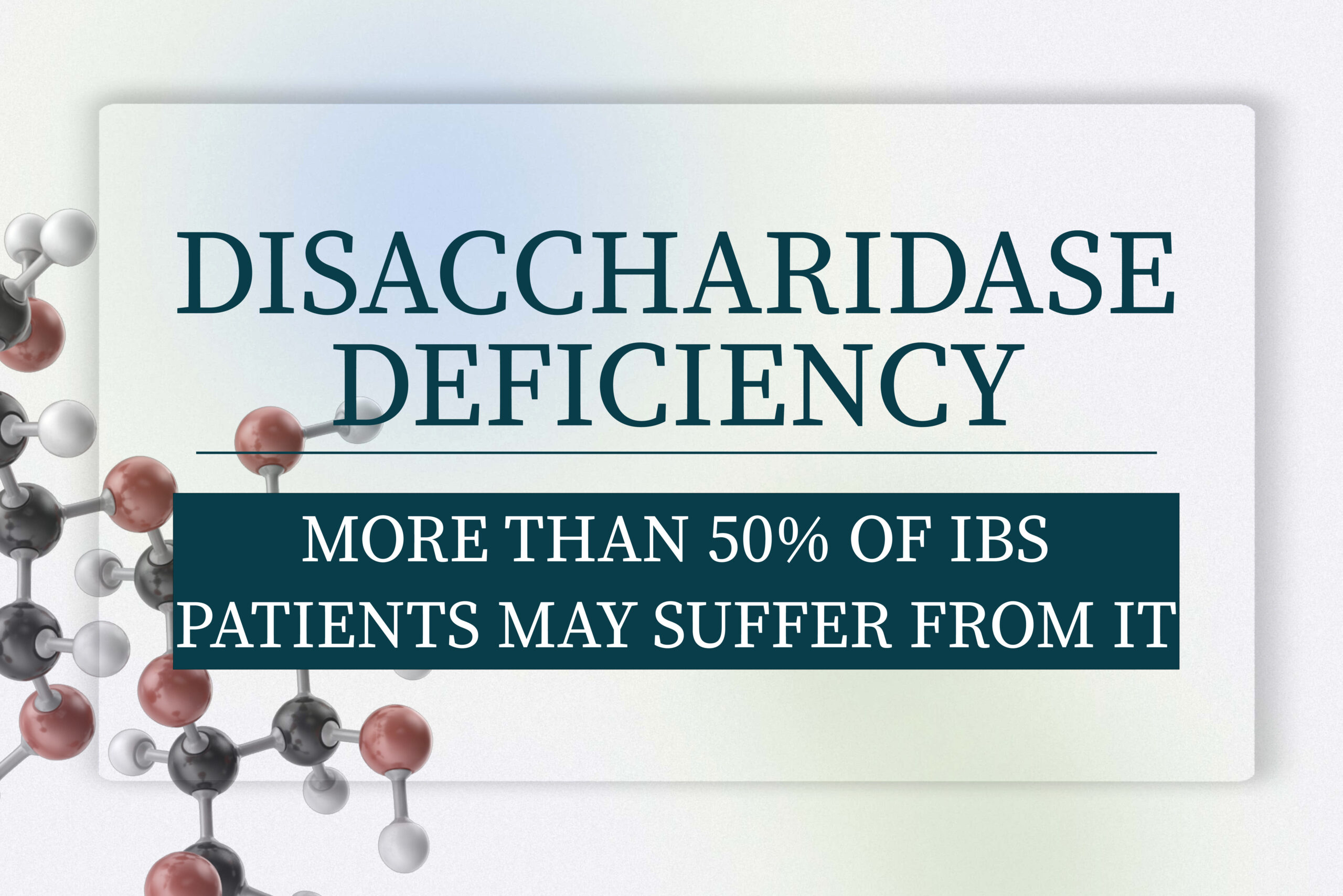
A 2023 study found that almost half of the patients presenting with functional gastrointestinal symptoms may suffer from intestinal disaccharidase deficiency! That means that they over-ferment specific sugar molecules; and lactose is just one of them. Find out what causes it and how to test at-home.
Disaccharidase deficiency or irritable bowel syndrome?

IBSyncrasy
Every IBS is unique
Lactase deficiency, commonly known as lactose intolerance, where the body struggles to break down lactose, a sugar found predominantly in dairy products, might be familiar to you. However, a less-known but equally significant condition known as disaccharidase deficiency has been emerging in the medical field. Recent research points towards a higher prevalence of this condition in adults than previously assumed. Furthermore, this deficiency may often be obscured by Irritable Bowel Syndrome (IBS) symptoms, increasing the complexity of diagnosis and treatment.
Disaccharidase deficiency and gastrointestinal symptoms
- Lactase
- Sucrase
- Maltase
- Isomaltase

IBSyncrasy
Every IBS is unique
Disaccharidases play an indispensable role in carbohydrate digestion and absorption. These enzymes, produced within the intestinal brush border, simplify complex sugars into absorbable, simple sugars. Nevertheless, this process is disrupted in individuals with a disaccharidase deficiency.
The deficiency of these enzymes might seem a trivial setback in the vast landscape of digestive functions, but it is indeed a significant one. The deficiency has a direct effect on a person’s health, leading to gastrointestinal symptoms like chronic abdominal pain, gas, bloating, and diarrhea. Alarmingly, individuals deficient in all four disaccharidases, known as ‘pan-disaccharidase deficiency’, experience a more severe weight loss compared to those with a single disaccharidase deficiency.
The symptoms of disaccharidase deficiency show remarkable similarity to IBS, a prevalent gastrointestinal disorder affecting numerous individuals globally. It’s worth noting that some IBS sufferers might, in reality, be struggling with an undiagnosed disaccharidase deficiency.
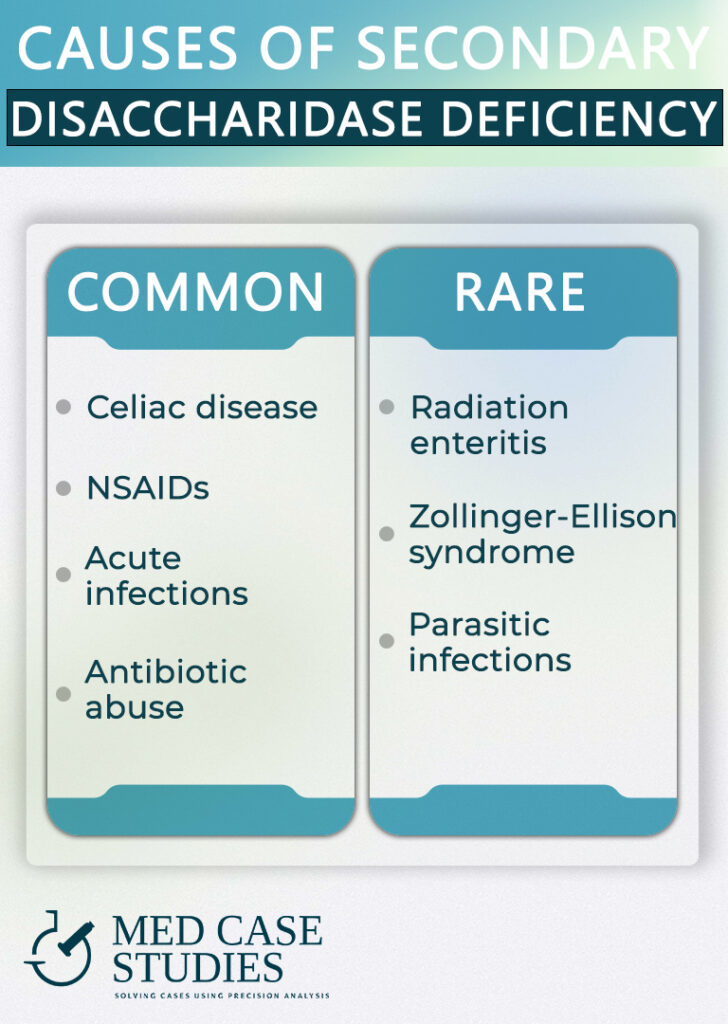
Different forms of disaccharidase deficiency

Eating behaviors and the gut microbiome
The average American consumes around 300 grams of carbohydrates and 140 grams of sugar daily. Within these, lactose and sucrose are the most prevalent. In the case of lactase non-persistence, a common phenotype in adults, your body decreases the production of lactase. This lactase deficiency can lead to diarrhea if lactose intake exceeds the gut’s absorption capacity.
The enzyme sucrase has a crucial function in decomposing sucrose into glucose. This enzyme, together with isomaltase, stems from the Sucrase-Isomaltase (SI) gene. A functional variant in this gene can cause sucrose and starch intolerance, known as congenital sucrase-isomaltase deficiency (CSID), an autosomal recessive disorder. Fascinatingly, these variants in the sucrase-isomaltase gene are detected more frequently in IBS patients, creating an interesting connection between disaccharidase deficiency, carbohydrate malabsorption, and IBS.
Primary or secondary

7 tips for faster PI-IBS
recovery time
Diagnosing disaccharidase deficiency in patients
Post Infectious IBS
Success case study
Considering the significant symptom overlap between disaccharidase deficiency and IBS, how can one accurately diagnose these conditions?
The solution resides in a combination of small intestinal biopsies and breath tests. Duodenal biopsies, minute tissue samples from the duodenum — the first part of the small intestine — are recognized as the standard for identifying disaccharidase deficiency. Nonetheless, breath tests offer an invaluable, non-invasive diagnostic tool. Patients with disaccharidase deficiency exhibit certain changes in their breath after sugar consumption, further validating the diagnostic process. Disaccharidase testing using methods like the Dahlqvist method and disaccharidase assay further aids the diagnosis, thereby leading to better diagnosis and treatment outcomes.
This highlights the significance of disaccharidase deficiencies in children and adults alike and the need for early diagnosis to prevent the risk of irritable bowel syndrome and chronic abdominal pain. The crucial role of genetic testing is also underscored to detect the increased risk of irritable bowel syndrome in patients with functional variants in the sucrase-isomaltase gene.
Check disaccharidase deficiency at home
Perform this test and find out
The intricacies of diagnosing disaccharidase deficiency call for a systematic, empirical approach. Owing to the symptomatic overlap between this condition and other gastrointestinal disorders like IBS and celiac disease, it becomes paramount to employ a method that can differentiate between these conditions while diagnosing accurately. The prevalence of disaccharidase deficiencies demands a technique that is both comprehensive and precise. The following steps offer an empirical approach to diagnosing disaccharidase deficiencies, focusing on the individual’s reaction to dietary modifications. These steps align with the objective of detecting disaccharidase levels and identifying specific enzyme deficiencies.
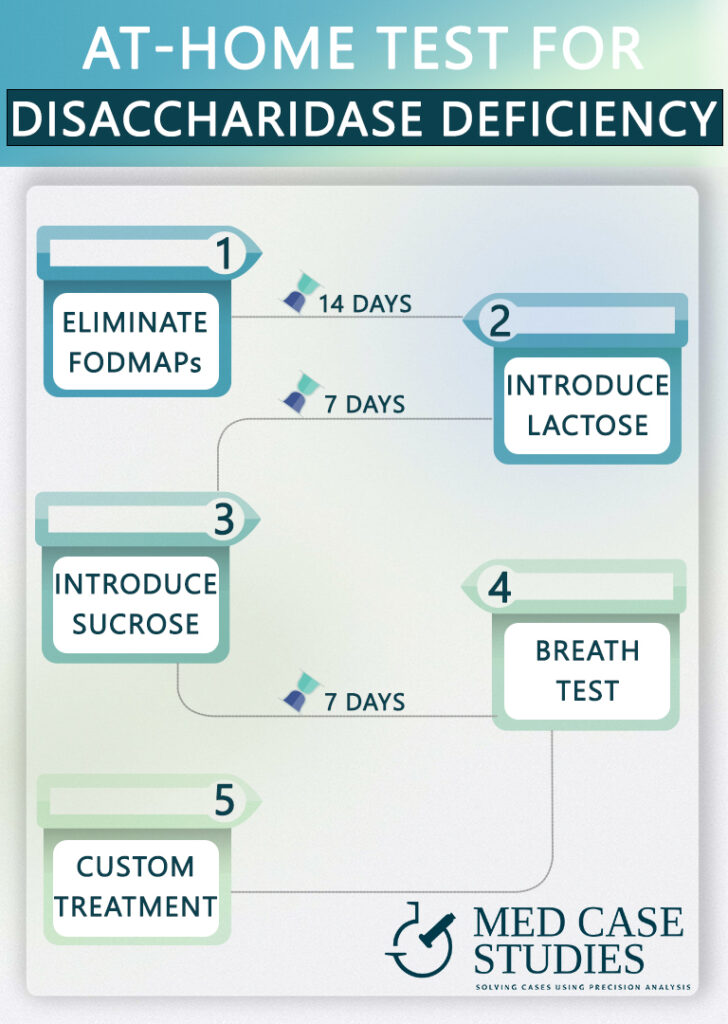
The steps are:
Eliminate FODMAPs: Start by adopting a low FODMAP diet. This dietary approach is frequently utilized to ease symptoms associated with Irritable Bowel Syndrome (IBS) and might be effective in mitigating symptoms related to disaccharidase deficiencies, including pan-disaccharidase deficiency.
Reintroduce Lactose: 14 days later, reintroduce lactose into your diet. Not too much, just 1/2 glass of milk for 7 days will suffice. If symptoms resurface or exacerbate, it could signal a lactase deficiency, a form of disaccharidase deficiency.
Reintroduce Sucrose: Subsequently (after 7 days), reintroduce sucrose into your diet. If symptoms reappear or worsen upon this reintroduction, this could be indicative of a sucrase deficiency, pointing towards a possible sucrase-isomaltase deficiency.
Perform a Breath Test: If the reintroduction of lactose and sucrose triggers symptoms, it would be prudent to discuss undergoing the 13C-Sucrose Breath Test with your healthcare provider. This non-invasive test can provide crucial insights into potential disaccharidase deficiency, thus proving instrumental in the diagnostic process.
Consult with a Healthcare Provider: If the breath test indicates disaccharidase deficiency, consult with your healthcare provider for appropriate next steps. These could entail enzyme replacement therapy or further dietary modifications to manage symptoms. In some cases, an endoscopy may be recommended to better understand the condition and devise an effective treatment strategy.
FAQ
How is disaccharide deficiency treated?
Treatment for disaccharidase deficiency hinges on an individual’s specific enzyme deficiency, employing a mix of enzymes and dietary modifications. Levels of deficiency dictate dietary restrictions. Post-antibiotic treatment often necessitates further adaptations due to reduced enzyme levels.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.