The gut microbiome and systemic sclerosis:
A new connection unveiled
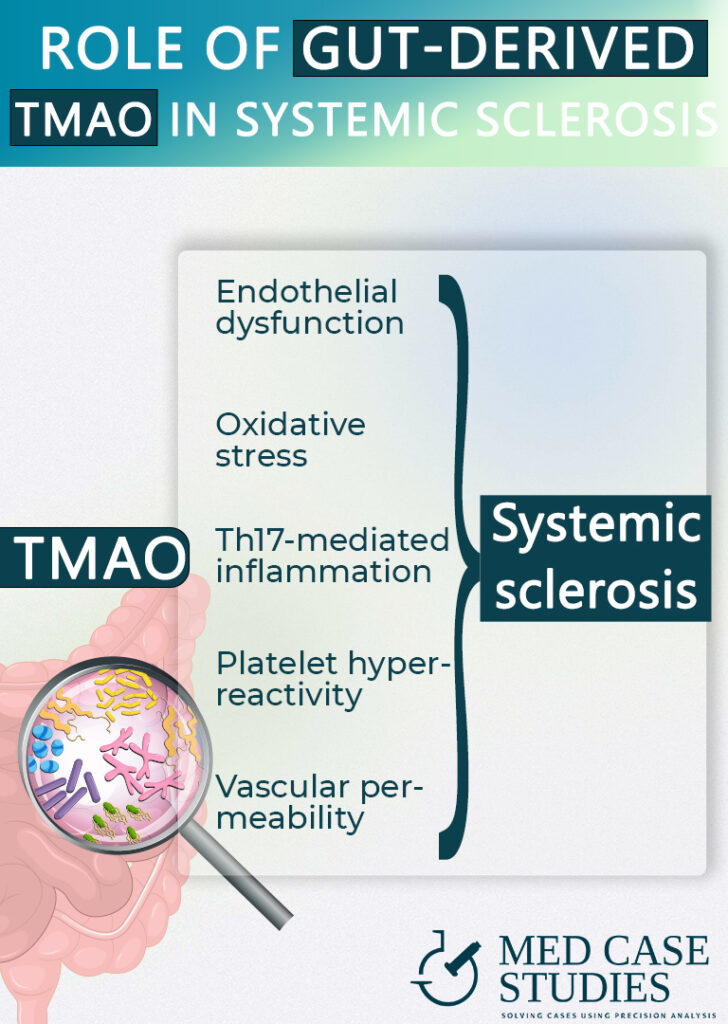
Trimethylamine N-Oxide, a gut microbial metabolite produced mainly after consumption of red meat, may be linked to complications in systemic sclerosis patients
Microbiota in SSc: The connection between gut microbiome and systemic sclerosis

IBSyncrasy
Every IBS is unique
Systemic sclerosis (SSc), also known as scleroderma, is a rare autoimmune disease affecting connective tissues, causing fibrosis in the skin and internal organs. The exact cause remains unclear, and there is a lack of established biomarkers to determine its severity and gastrointestinal involvement. Recently, researchers have explored the connection between gut microbiota and SSc, specifically examining the role of gut bacteria and their metabolites in the development and progression of the disease. A new study published in the Journal of Inflammation Research has discovered a potential link between a gut microbial metabolite, Trimethylamine N-Oxide (TMAO), and specific complications in systemic sclerosis patients.
The role of TMAO in scleroderma complications

IBSyncrasy
Every IBS is unique
The study aimed to determine the concentration of TMAO in patients with systemic sclerosis and its possible correlation with certain manifestations of the disease, including gastrointestinal symptoms. According to lead researcher Albert Stec, “Our findings reveal that TMAO concentration is significantly increased in systemic sclerosis, particularly in patients with advanced gastrointestinal involvement. This is the first study evaluating plasma TMAO in systemic sclerosis, and our results suggest that bacterial metabolites may represent a link between gut microbial dysbiosis and organ involvement in the disease.”
Researchers used high-performance liquid chromatography to measure TMAO concentration in 63 SSc patients and 47 matched control subjects. The study analyzed the correlation between TMAO concentration and markers of heart involvement (left ventricle ejection fraction, NT-proBNP), a marker of interstitial lung disease (ILD) severity, and the Scleroderma Clinical Trials Consortium Damage Index.
The study found that plasma TMAO levels were significantly higher in systemic sclerosis patients (283.0 ng/mL) compared to the control group (205.5 ng/mL). Moreover, increased TMAO concentrations were observed in patients with concomitant ILD and gastrointestinal tract dysmotility, two complications associated with systemic sclerosis. These results suggest that TMAO may play a role in the development or progression of specific complications in patients with systemic sclerosis.
Can the gut microbiome be modified in systemic sclerosis patients?

IBSyncrasy
Every IBS is unique
It is early for a definite answer, but it seems promising. While this study provides valuable insights into the potential link between TMAO and SSc complications, other studies have focused on different aspects of gut microbiome in systemic sclerosis. For example, some research has explored the role of probiotics or fecal microbiota transplantation in improving gastrointestinal symptoms of SSc. These complementary findings emphasize the importance of considering multiple sources of information when examining the relationship between gut microbiota and systemic sclerosis.
Healthy gut microbiota for systemic sclerosis
 Mediterranean diet for gut microbiome
Mediterranean diet for gut microbiomeNow what?

Actionable tips
- Consume early dinners and seasonal vegetables to reduce TMAO-induced endothelial dysfunction and fibrosis in systemic sclerosis, addressing gut dysbiosis and promoting a balanced gut microbiota.
- Drink antioxidant-rich herbal tea and use healthy cooking methods to counteract TMAO-induced oxidative stress, inhibiting inflammation and vascular damage in systemic sclerosis, while supporting gut microbiome balance.
- Supplement with Lactobacillus rhamnosus GG probiotics to mitigate Th17-mediated inflammation in systemic sclerosis, modulating gut microbiota, reducing TMAO production.
- Implement regular vegetarian days with seasonal vegetables to decrease TMAO levels, reduce platelet hyperreactivity, and lower thrombotic risk in systemic sclerosis, improving the imbalanced gut microbiome and the role of gut microbiota.
- Favor the role of gut microbiota in systemic sclerosis by consuming salad with meat and practicing intermittent fasting, attenuating TMAO-induced endothelial cell activation, vascular permeability, and pro-inflammatory cytokine release, while enhancing gut microbiome balance.
FAQ
Is there a role for the microbiome in systemic sclerosis?
Yes, there is a role for the microbiome in systemic sclerosis. The study found that Trimethylamine N-Oxide (TMAO), a gut microbial metabolite, is significantly increased in patients with systemic sclerosis, particularly those with advanced gastrointestinal involvement. This suggests that bacterial metabolites like TMAO may contribute to the pathogenesis of systemic sclerosis and its complications.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.