
SIBO-related IBS. The only book that provides treatment based on years of clinical experience
Small Intestinal Bacterial Overgrowth (SIBO) is a condition where an excessive number of bacteria colonize the small intestine, disrupting the natural balance of the gut microbiome. This imbalance can lead to a variety of frustrating digestive symptoms and health issues. But, every bacterium causing small intestinal bacterial overgrowth has different metabolic traits and causes SIBO differently.

Successful SIBO - IBS Case Study
SIBO is typically categorized based on the type of gas produced by the overgrown bacteria in the duodenum or jejunum: hydrogen, methane, or hydrogen sulfide. The specific gas present can provide insights into the type of bacteria causing the overgrowth and help guide treatment options.
Hydrogen-producing SIBO (H2-SIBO): In this type, bacteria like Escherichia coli, Klebsiella, and Enterobacter produce hydrogen as a byproduct of fermenting carbohydrates. H2-SIBO is often associated with diarrhea-predominant symptoms.
Methane-producing SIBO (Me-SIBO): Methanobrevibacter smithii, a type of archaea, consumes the hydrogen produced by other bacteria and generates methane. Me-SIBO is commonly associated with constipation and slower gastrointestinal motility.
Hydrogen sulfide-producing SIBO (H2S-SIBO): This form of SIBO involves bacteria like Desulfovibrio piger, which produce hydrogen sulfide as a byproduct of their metabolism. Hydrogen sulfide SIBO can lead to symptoms such as bloating, gas, and diarrhea.
Following our discussion on small intestinal bacterial overgrowth, it is important to recognize the signs and symptoms of this condition, as well as the risk factors that can increase the likelihood of developing SIBO
The symptoms of SIBO can vary depending on the type of gas produced by the bacteria in the small intestine (hydrogen and methane), but common symptoms include bloating, gas, constipation, diarrhea, belching, and pruritus (itching). These symptoms can significantly impact a person’s quality of life, affecting their social interactions, work performance, emotional well-being, and overall health.
For example, the abdominal pain and bloating associated with overgrowth of bacteria in the small intestine can cause discomfort and embarrassment, leading to social withdrawal and isolation. Additionally, the unpredictable nature of diarrhea and constipation can make it difficult for individuals to manage work and daily activities, increasing stress and anxiety. The chronic nature of SIBO symptoms can also lead to fatigue and a general sense of malaise, further impacting emotional well-being and overall health.

Proton pump inhibitors abuse and IBS
Case Study
There are several predisposing factors that can increase the likelihood of developing SIBO, including:
Proton pump inhibitors (PPIs): PPIs are commonly prescribed medications for acid reflux and GERD. However, long-term use of PPIs can alter the acidity of the stomach, allowing for the overgrowth of small intestine bacteria.
Diabetes: Individuals with diabetes, particularly those with poorly controlled blood sugar levels, are at an increased risk of developing bacterial overgrowth due to slower gastrointestinal motility and impaired immune function.
Frequent snacking: Eating small meals or snacking frequently throughout the day can inhibit the normal functioning of the Migrating Motor Complex (MMC), a process responsible for sweeping residual food and bacteria through the digestive tract. This disruption can lead to bacterial overgrowth in the small intestine.
Cholecystectomy: The removal of the gallbladder can alter the release of bile into the small intestine, which may disrupt the balance of gut bacteria and increase the risk of SIBO.
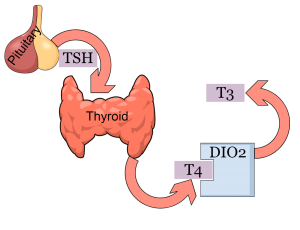
Hashimoto's and IBS
Case Study

While understanding the signs and symptoms of Small Intestinal Bacterial Overgrowth is crucial, the process of identifying and treating this condition can be challenging.
SIBO is usually diagnosed through a breath test, which is considered the gold standard for detecting the presence of hydrogen or methane gases in the breath. The test measures the gases produced by bacteria in your small intestine as they ferment carbohydrates. During the test, patients ingest a sugar solution, such as lactulose or glucose, and their breath is analyzed at regular intervals. An increase of more than 20 ppm H2 within the first 1-1.5 hours is considered positive for SIBO, while an increase of more than 10 ppm methane or hydrogen sulfide is also indicative of the condition.
The breath test, while useful, has its limitations. It only provides an approximation of the site of SIBO and its gas product, rather than identifying the specific bacteria responsible for the condition. Furthermore, it doesn’t give information on the specific metabolic needs of the bacterial culprit or its sensitivities to antibiotics or natural treatments, such as berberine, garlic, or oregano.
When it comes to SIBO treatment using only this information, the same approach is often prescribed regardless of the bacteria involved: antibiotics (usually rifaximin), sometimes accompanied by prokinetic agents (natural or pharmaceutical), and nutritional advice. Some practitioners may also recommend probiotics, although the evidence supporting their use in treating SIBO is mixed.
Given these limitations, relying solely on breath tests may not provide the most effective treatment for SIBO patients. To truly understand and address the underlying causes of bacterial overgrowth, it’s essential to identify the specific overgrown bacterial populations and additionally delve deeper into an individual’s symptoms and medical history, in order to formulate a custom and effective treatment.

As we’ve discussed, traditional diagnostic methods for Small Intestinal Bacterial Overgrowth have their limitations. Duodenal aspiration offers several advantages that can lead to more effective treatment plans. By taking fluid from the small intestine, a doctor may identify the specific bacteria responsible for a patient’s SIBO which is crucial for successful treatment. In this section, we’ll explain why knowing the specific microorganism that produced SIBO is essential and how it can lead to more effective treatment plans.
Sensitivity testing: By knowing the exact bacterium leading to SIBO, healthcare practitioners can perform sensitivity testing to determine which antibiotic or natural substance the bacteria are susceptible to. This is especially important when using natural substances, as patients can take them daily without side effects, ensuring long-term remission of symptoms.
Determining the underlying cause: Identifying the specific bacterium responsible for SIBO can help determine why it developed in the first place. For example, if Fusobacterium is found in the small bowel, periodontitis can be investigated as a potential cause. In the case of E. coli, the consumption of undercooked meat could be a contributing factor.
Personalizing the diet: Adjusting a patient’s diet based on the specific metabolic preferences of the SIBO-causing bacterium can enhance treatment effectiveness. For instance, if Klebsiella is the culprit, a starch-free diet for a few weeks will ensure success.
Making informed decisions about probiotics: Knowing the specific bacterium leading to SIBO can guide the decision to use probiotics and which strains to use. If SIBO is caused by a Lactobacillus strain, then Lactobacillus supplementation should be avoided during treatment.
Avoiding harmful supplements: Identifying the specific bacterium can help avoid supplements that may inadvertently promote the growth of harmful microorganisms, in addition to beneficial ones.
Several microorganisms are commonly associated with small intestinal bacterial overgrowth. Understanding their specific mechanisms of causing pathology when overgrown in the small intestine can help in developing targeted treatment strategies.
Enterococcus faecalis: Overgrowth of this bacterium can disrupt the delicate balance of the gut microbiome, leading to a weakened immune system and increased susceptibility to infections.
Lactobacillus spc: Overgrowth of certain Lactobacillus species can produce lactic acid, which can irritate the gut lining and impair proper digestion.
Proteus spc: When overgrown in the small intestine, Proteus species can produce urease, an enzyme that increases the pH of the gut, making it less hospitable for beneficial bacteria and causing digestive issues.
Fusobacterium: Overgrowth of Fusobacterium can contribute to the formation of biofilms in the small intestine, which can impede nutrient absorption and disrupt normal bowel function
Microorganism | Trait | Specific intervention |
|---|---|---|
E. coli | Production of endotoxins | Intake of natural endotoxin inhibitors |
Klebsiella pneumoniae | Increased amylase activity | Low starch diet |
Enterococcus faecalis | Disruption of gut microbiome balance | Intake of specific bacteriophage therapy targeting Enterococcus faecalis |
Lactobacillus spc | Production of lactic acid | Abstinence from probiotics for at least 2 months |
Proteus spc | Swarming in presence of excess glutamine | Glutamine avoidance |
Fusobacterium | Formation of biofilms in the small intestine | Increased intake of natural biofilm disruptors, such as curcumin |
Certainly not. Stool tests are often used to diagnose disorders of the large bowel, but they fall short when it comes to detecting small intestinal disorders like SIBO. Stool tests lack sensitivity and can lead to guesswork in identifying the specific bacteria responsible for SIBO. For example, elevated levels of Desulfovibrio in a stool test might suggest H2S-SIBO, but this is not always the case.
One reason for the inadequacy of stool tests in diagnosing SIBO is that the small and large intestines have different microbiomes. The small intestine has a lower bacterial count and different bacterial composition compared to the large intestine. Stool tests mainly analyze the large intestine’s microbiome, which may not accurately reflect the bacterial populations in the duodenum and jejunum. Furthermore, the transit time and bacterial degradation of the stool sample can lead to misleading results.
SIBO-causing bacteria often complete their life cycle in the small intestine, which is why lipopolysaccharides (LPS) can enter the circulation. However, obtaining a sample from the duodenum is not an easy task. In cases where a gastroscopy is performed, a specific sample can be requested for analysis to get a more accurate diagnosis.
Another limitation of PCR-based stool tests is their inability to differentiate between live and dead bacteria. This can be problematic because the presence of dead bacteria does not necessarily indicate small intestinal overgrowth. Additionally, stool tests may not accurately identify the metabolic activity of the bacteria, which is crucial in understanding the severity and impact of SIBO on the patient’s health.
Knowing the specific bacterium in your gut that is responsible for SIBO through duodenal aspiration allows the tailoring of effective treatment plans. This individualized approach can include medical interventions such as antibiotics and prokinetics, dietary adjustments like the elemental diet or low-FODMAP diet, and lifestyle modifications such as intermittent fasting and chrononutrition.
Antibiotics are chosen based on the sensitivity testing results, ensuring that the selected medication effectively targets the specific bacteria causing the overgrowth. Prokinetics help improve motility in the small bowel, preventing further bacterial overgrowth and soothing gut symptoms. Dietary interventions, like the elemental and low-FODMAP diets, focus on limiting fermentable carbohydrates that could exacerbate bacterial growth. These diets may be recommended after the tests suggest SIBO and based on the test’s results.
With a comprehensive and customized approach based on the specific bacterial strain responsible for the overgrowth, supplementary treatments, including, prebiotics, and mucosal nutrients will be highly personalized. Antimicrobials may be used to target specific bacterial strains causing SIBO, further enhancing the treatment’s efficacy.
Additional interventions may be implemented depending on the type of bacteria identified. For example, if an oral pathogen is the culprit, improving oral hygiene may be recommended. If the SIBO cause is a Proteus strain, glutamine avoidance might be suggested as part of the treatment strategy.
Addressing overall digestive health is crucial when treating SIBO, as it can help to prevent the recurrence of the condition. A focus on proper nutrient absorption is also essential, as SIBO can lead to vitamin deficiencies. Maintaining a balanced sibo diet and understanding the importance of small intestinal bacterial overgrowth management can contribute to long-term digestive health.
In conclusion, my experience with SIBO has shown that a personalized approach to treatment is key to achieving full recovery and maximum symptom improvement. Although only 1 in 10 SIBO cases in my practice have duodenal aspiration data, those patients who do undergo this diagnostic procedure benefit significantly from the tailored treatments and diets provided. By identifying the specific bacterial strains causing the overgrowth and designing a targeted intervention plan, we can address the root cause of the condition and work towards a long-lasting resolution of symptoms. Implementing custom treatments and diets, alongside medical interventions and lifestyle adjustments, has proven to be an effective way to help patients overcome SIBO and therefore regain their quality of life.
Yes, the SIBO test (hydrogen breath test) is fairly reliable in identifying bacterial overgrowth. However, it only provides an approximation of the extent and location of SIBO, and may produce false positives or negatives.
First signs of SIBO include gut symptoms like bloating, gas, indigestion, GERD, and abdominal pain, as well as skin symptoms such as pruritus, eczema, and erythema. These symptoms often result from bacterial overgrowth disrupting normal digestion.
Strange symptoms of SIBO include fatigue, irritability, brain fog, increased pain sensitivity, joint pain, and nutritional deficiencies. These symptoms occur as bacterial overgrowth affects nutrient absorption and may cause systemic inflammation.
Erdogan, Askin, et al. “Small intestinal bacterial overgrowth: duodenal aspiration vs glucose breath test.” Neurogastroenterology & Motility 27.4 (2015): 481-489.

| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checkbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checkbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |