Vegan IBS
IBS after antibiotics for UTI. 23 y.o. vegan girl

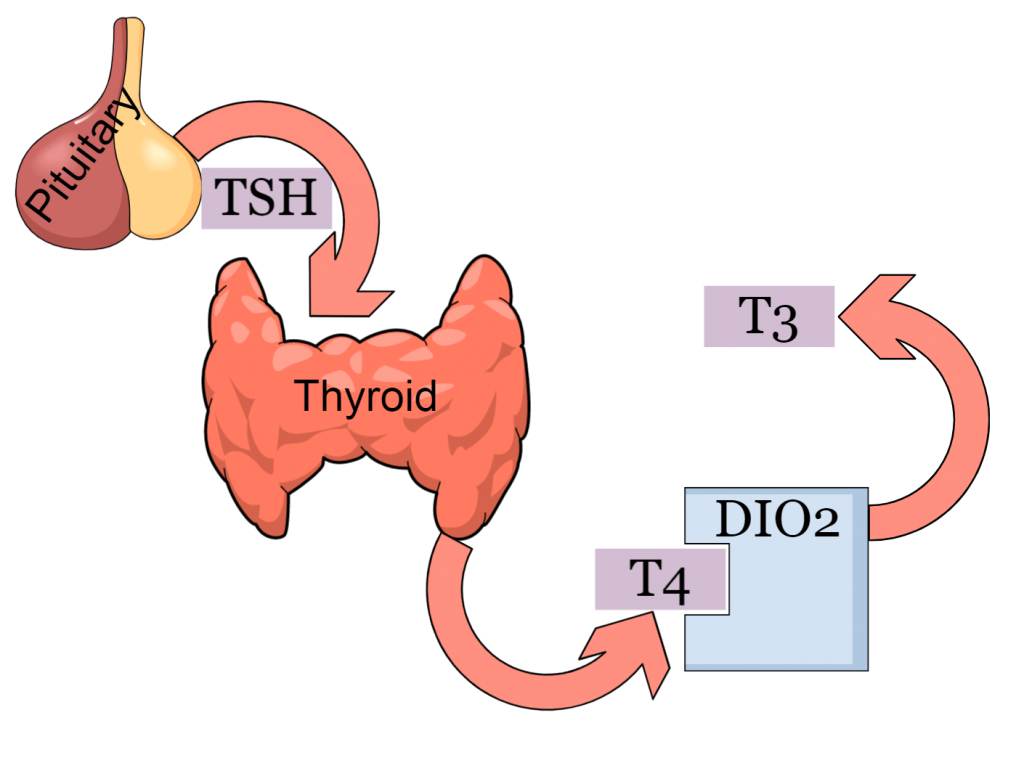
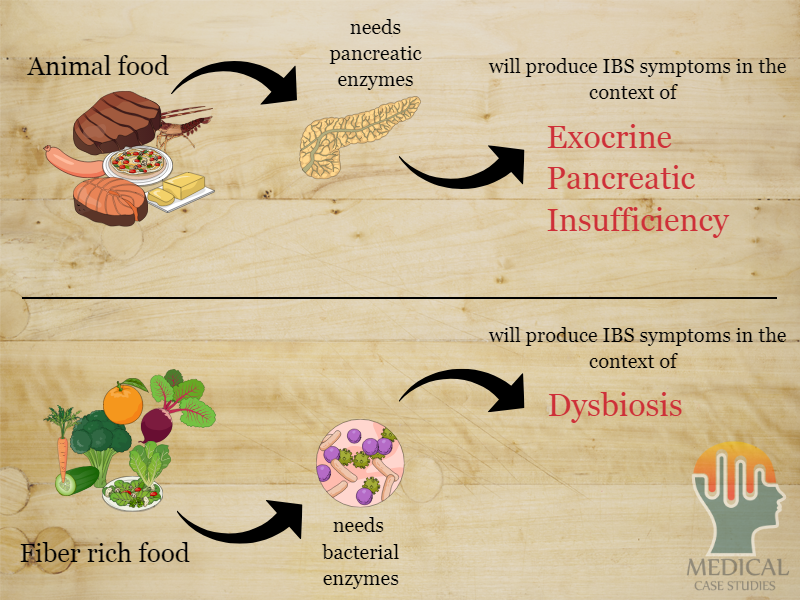
Our pancreas possess amylases, proteases and lipases. Not cellulases, not xylanases. We have others to do this job for us. Several trillions of others, right inside our gut. Our gut bacteria possess many enzymatic activities, which may degrade fiber, in favor of both themselves and the host (us). But we need them to be there when fiber goes down the colon and their diversity should be optimal. In addition, it is not uncommon for vegans to produce less pancreatic enzymes. This is natural since they need less of them. But when they eat something very fatty, their lipase content should be adequate.
Walkowiak, Jaroslaw, et al. “Vegetarian diet alters the assessment of exocrine pancreatic function with the use of fecal tests.” Journal of pediatric gastroenterology and nutrition 38.2 (2004): 224-226.
Walkowiak, Jaroslaw, et al. “Adaptive changes of pancreatic protease secretion to a short-term vegan diet: influence of reduced intake and modification of protein.” British Journal of Nutrition 107.2 (2012): 272-276.
Walkowiak, Jaroslaw, et al. “The elimination of meat from the diet selectively decreases pancreatic elastase secretion.” British journal of nutrition 98.1 (2007): 154-158.
Jenny was a 23 years old very beautiful girl who visited my office on January 2017. She had just accepted her first job in a big marketing company whereas she was already working as a fashion model. This side kick job was the main reason why the first thing she asked me to help her with was bloating and lower abdominal pain. Her medical history begun 7 years ago when she experienced her first UTI. During the next 7 years UTI’s recurred at least once per year and as a result she had taken tons of antibiotics. 2 years ago, after another urinary tract infection and the corresponding antibiotic treatments she felt extremely bloated, during a photoshoot. This symptom resolved on its own several hours later. From that point on she never had a normal bowel movement again. Her stool was constantly loose and occasional incidents of diarrhea were the new normal. She woke up bloated on a daily basis usually with a moderately intense hypogastric pain. In addition, Jenny would get much worse a few days before menstruation, whereas sometimes the symptoms insisted throughout the whole month. In the mean time she had visited 2 gastroenterologists who prescribed her with spasmolytics and probiotics. Both times she experienced a mild improvement but nothing worked for longer than a month. The last time she saw her doctor he mentioned antidepressants and relaxation. She never went back. Jenny was not depressed, neither stressed.

One thing, not properly evaluated in her health history was the fact that ever since she was 18, Jenny was vegan. And vegan means fiber, lots of fiber. In fact, almost every vegan meal is full of fiber.
The pain located under the belly button is most of the times attributed to accumulated air and pathologic fiber fermentation
Loose stool is a sign of increased water and mucus excretion inside the colon, in order to get rid of indegested fiber
Extensive fiber fermentation produces vast amounts of gas, resulting in bloating
The more fiber ingested, the better the microbiome composition should be. But Jenny had bombed her microbiome with at least 150 antibiotic pills in total. And she followed a diet pattern that needs super gut microflora, in order to avoid symptoms. All these antibiotics had produced a low-quality bacterial content diminishing the capability of commensal fiber-degraders to process fiber properly. So the extra amount of fiber that reached Jenny’s colon lead to abnormal fermentation processes and enhanced gas production. That’s how bloating and lower abdominal pain were explained. In addition, her exocrine pancreatic output was lower than expected for her age 280 mg/g stool but still within the normal range. Also, elevated concentrations of Candida albicans could also explain the amounts of gas produced as well as the vaginosis. Lastly, Klebsiella pneumoniae and Escherichia coli were detected in large amounts. These two bacteria were also isolated from past urinary cultures during testing for urinary tract infections.
C. difficile toxin A
This toxin was recovered in medium amounts and could be attributed to the multitude of antibiotics Jenny had consumed
Klebsiella/E. coli
Both pathogens in large amounts may explain loose stool and frequent UTI’s
Low elastase for her age
This value is reversible and usually, in the absence of diabetes or other metabolic disorders, it is attributed to veganism
Probiotic sterility
Not a sign of Lactobaciili or Bifidobacteria. Fibers are underdegraded and overproduce air
Candida albicans
Fungi having many enzymatic properties which use sugars as substrate. This leads to alcoholic fermentation of sugars and a lot of gas
Jenny’s treatment was multi-disciplinary. Besides taking care of her exhausted commensal microorganism (both in pro- and pre-biotic manner) pathogenic microorganisms needed separate antimicrobial treatments. One antibacterial and one antifungal. A broad spectrum antimicrobial treatment was thus given along with a proper enzyme supplement. Diet in these cases is challenging, because the meals are limited to non animal ones.

Jenny’s dysbiosis was an extensive one. Too many years with antibiotics and gradual microbiome destruction. Even after full recovery caution should be undertaken and every new antibiotic should be accompanied with proper probiotic treatment. Vegan, being a good diet in comparison to the western ones confers several restrictions. The efficacy of the treatment is not compromized, it just takes longer for full recovery to be achieved. In Jenny’s case, full recovery was achieved about 4 months later.
- Being vegan for over a year confers a reduction in exocrine pancreatic output, at least for elastase and chymothrypsin
- Vegan diets may be more compatible to our microbiome but any deviation from optimal may bring IBS symptoms to the surface
- Multiple antibiotics perturb the diversity and quality of gut microbial populations
- Bloating, gas and pain are the commonest symptoms, whereas women are more prone to this kind of IBS
- Choices in lifestyle and diet play a decisive role in the way in which dysbiosis will manifest

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.