Secretory IgA IBS
Chronic infections and IBS. The crucial role of low sIgA levels
Number of cases
Mean age
Rate of success
Treatment duration
Most common symptom
Most common culprit
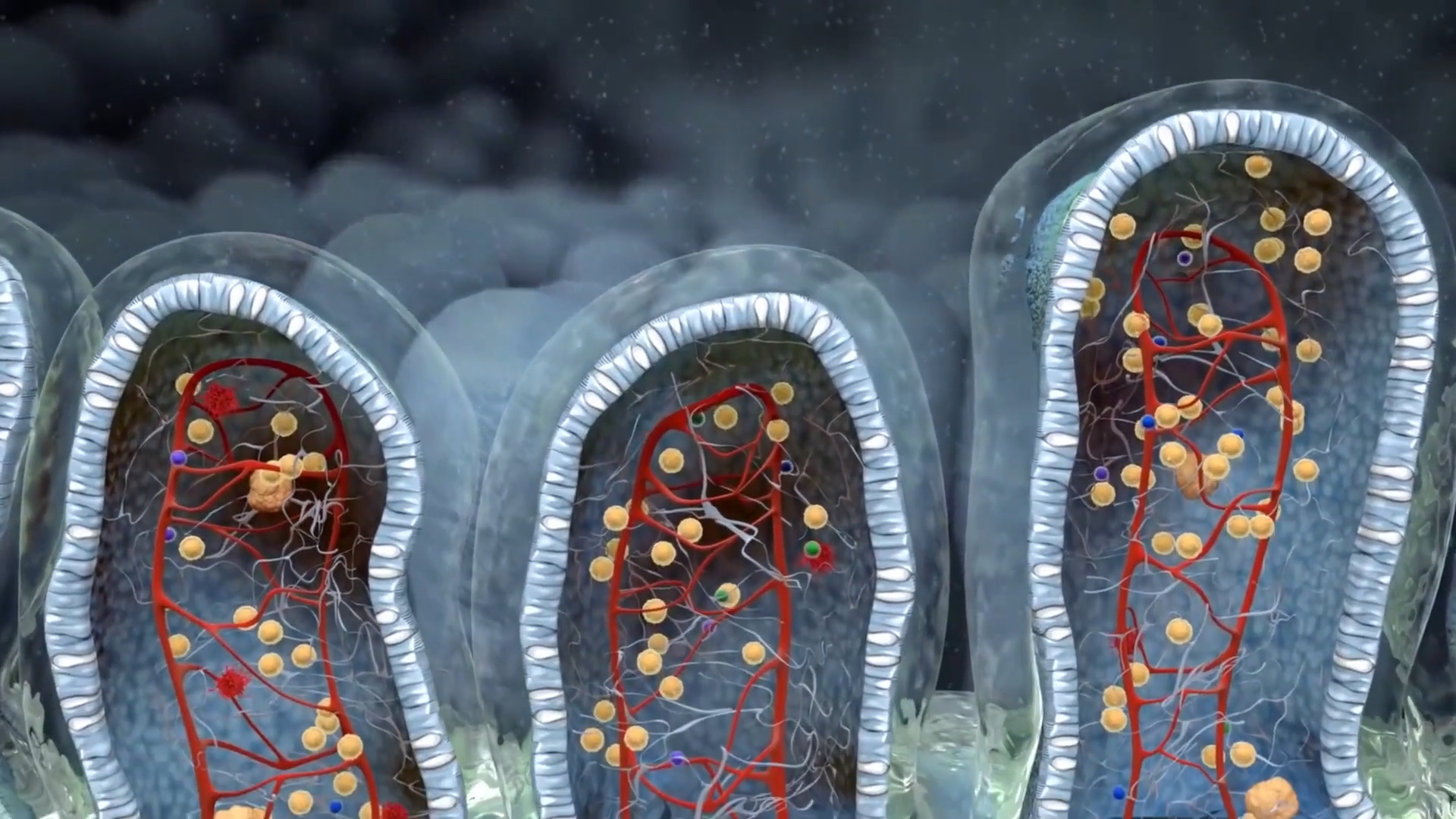
In addition to this crucial function, sIgA plays several other vital roles, including modulating our microflora in a direct way, regulating the allergenic potential of a molecule, and presenting antigens to the immune cells to establish immunity. Because sIgA is the first and main line of defense in our intestinal system, sIgA deficiency can be a significant factor in the development of certain types of IBS.
Role in many diseases
Antibiotic abuse |
Eczema |
Allergies |
Chronic infections |
Psoriasis |
Rheumatoid arthritis |
Lupus |
Chronic infections and IBS can significantly impact one’s health, as evidenced by Mary’s case. Mary, a 39-year-old nurse and mother of two, has worked in hospitals for the past 18 years. Despite receiving regular vaccinations, Mary frequently falls ill with symptoms such as low-grade fevers, upper respiratory infections, urinary tract complaints, and gastroenteritis. Initially, Mary attributed her frequent illnesses to the hospital environment. However, she soon realized that her colleagues did not experience the same level of sickness.
As a result, Mary began consuming a large number of antibiotics to combat her symptoms. Her cultures always tested positive for bacteria such as E. coli and Klebsiella pneumoniae. Unfortunately, after giving birth to her second daughter, Mary’s health took a turn for the worse. For the last 16 months, she has battled with gastrointestinal distress on a daily basis. Despite the medical treatment and lifestyle changes, her symptoms have persisted.
The first but most important event for proper sIgA production is the first contact of our gut with the "outside" micriobial world. C-section born babies exhibit different micobial signatures than vaginal born babies.
Adequate breastfeeding is crucial for immune maturation. Inadequate supply of maternal sIgA leads to late priming of MALT and diminished production of host IgA antibodies
GALTectomy (appendectomy and tonsillectomy) significantly decreases secretory IgA levels in serum. The decrease is more intense when both operations have been done
Mary's working environment exposes her to an increase burden of bacteria, viruses and fungi, thereby making her vulnerable to chronic infections

To begin, a systemic IgA deficiency test was ordered to confirm the role of sIgA in her symptoms. Other antibodies, including IgG, IgM, and IgE, were also tested to rule out any other potential culprits. While previous exams showed only a minor increase in her IgM titer, indicating chronic infection, it was important to consider all possibilities.
Given Mary’s extensive history of antibiotic use and exposure to hospital environments, a full 16sRNA stool test was ordered to assess the status of her microflora. It was important to understand how these factors may have altered her gut microbiome and contributed to her symptoms.
Furthermore, a Th1/Th2 balance blood test was ordered, along with several immune and biochemical biomarkers in stool. These tests would provide a comprehensive picture of Mary’s immune system and help identify any imbalances or deficiencies that may be contributing to her chronic infections and IBS.
Since fever was never above 38o C, the problem can’t be about the reaction capabilities of the immune system. Perhaps it is the first line of defense which cannot block out newly contacted pathogens, efficiently
The removal of tonsils has been implicated in many studies (human ones) in reducing sIgA production and in predisposing to frequent infections (mostly in mucosa coated organs)
While stress may exacerbate almost every human symptom, in this case there is also a direct biochemical link between stress and low sIgA. Cortisol, being the principle stress hormone, downregulates sIgA production worsening even more infectious predisposition. This is mostly true during the first 30 min of a stressful event
sIgA deficiency is an entity that cannot be “seen” but can be measured. It is also predictive of the affected organ (bronchoalveolar lavage for lungs, saliva for mouth, stool for gut)
Further testing showed that Mary was slightly Th1 dominant, and both C3 and C4 complement factors were marginally elevated. However, the 16sRNA stool test was alarming, revealing a massive dysbiosis with an abundance of gram-negative and gram-positive bacteria throughout her gut. This dysbiosis was a direct consequence of Mary’s prior heavy use of antibiotics and her lack of mucosal immunity.
In addition to these findings, Mary’s biochemical checkup revealed extremely low levels of vitamin D, vitamin B12, folic acid, iron, and ferritin. These deficiencies can contribute to chronic infections and IBS symptoms, as they can weaken the immune system and disrupt the body’s normal functioning. Finally, Mary’s salivary sIgA levels were detectable but fairly low, indicating further evidence of her sIgA deficiency.
sIgA deficiency
Undetected levels of sIgA mean that all opportunistic pathogens produce constant infectious inflammation explaining thereby Mary’s core symptoms
Heavy dysbiosis
This level of dysbacteriosis is deletetious to the mucosal immunity og the gut. Proper restoration is a prerequisite for sIgA production
Elevated complement factors
Constantly elevated complement factors mean that Mary’s immune reaction was always turned on, explaining the fatigue she encountered
Low salivary IgA
Salivary IgA is crucial in preventing foodborne and airborne infections. Proper oral immunity is considered very important
Paradoxically, the only way to start a successful treatment in this kind of case is another antibiotic course. The total bacterial load must be lowered before new probiotic inoculation and actions to increase sIgA content and production can be implemented.

On day 33 she visited my office again. She seemed very optimistic because her symptoms had not recurred but she did notice that bloating and multiple defecations appeared after night shifts. In general, bloating and mucus in her stools were minimized and so was the respiratory distress. Our next appointment was scheduled for after 45 days.
Given these challenges, individuals with sIgA deficiency must make a concerted effort to repair their mucosal linings and maintain sufficient sIgA levels to sustain a symptom-free status. While sIgA levels may never reach the levels of a non-predisposed person, lifestyle changes can make a significant difference in improving overall health and wellbeing.
To address sIgA deficiency, lifestyle changes such as diet, fasting, and good sleep habits are crucial and must be implemented for life. Before beginning treatment, healthcare providers must carefully inform patients that there may not be a permanent cure for their condition, and that lifestyle changes are an essential part of the total therapeutic regimen. In fact, supplements and drugs will only work effectively if they are implemented in conjunction with these lifestyle changes.
In summary, individuals with sIgA deficiency and chronic infections and IBS must take a proactive approach to their health, making lifestyle changes that can help repair their mucosal linings and sustain a symptom-free status. While there may not be a permanent cure, these changes can significantly improve overall health and wellbeing.
- sIgA deficiency is usually overlooked in IBS diagnoses. This is because it has been studied in the context of more serious diseases like autoimmune and cancer
- Lack of sIgA makes the pathogenicity of non commensal bacteria more prominent, giving rise to frequent infections of the gastrointestinal tract
- Bloating, loose stool and frequent diarrhea are the most comon symptoms, whereas other symptoms like nausea and vomiting are not uncommon
- sIgA replenishment is not an easy task and it usually takes time. Sometimes, the replenishment may reach up to marginally normal and no more. Genetic causes prevent it from achieving higher values
- Lifestyle choices play a determining role in sIgA production with anabolic stages (sleep, fasting etc) being very helpful in the process

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.