Chronic prostatitis and IBS - Success stories
Chronic bacterial prostatitis usually precedes the onset of IBS symptoms and may lead to pelvic pain syndrome
Number of cases
Mean age
Rate of success
Treatment duration
Most common symptom
Most common culprit
Men diagnosed with irritable bowel syndrome are much fewer in comparison with women. In fact, it seems that men almost always present with a commorbidity. Among the hundreds of male IBS cases, the most common comorbidity I have noticed is chronic prostatitis and chronic pelvic pain syndrome. In most of these cases, a prostatitis exacerbation is accompanied by a corresponding exacerbation of irritable bowel.
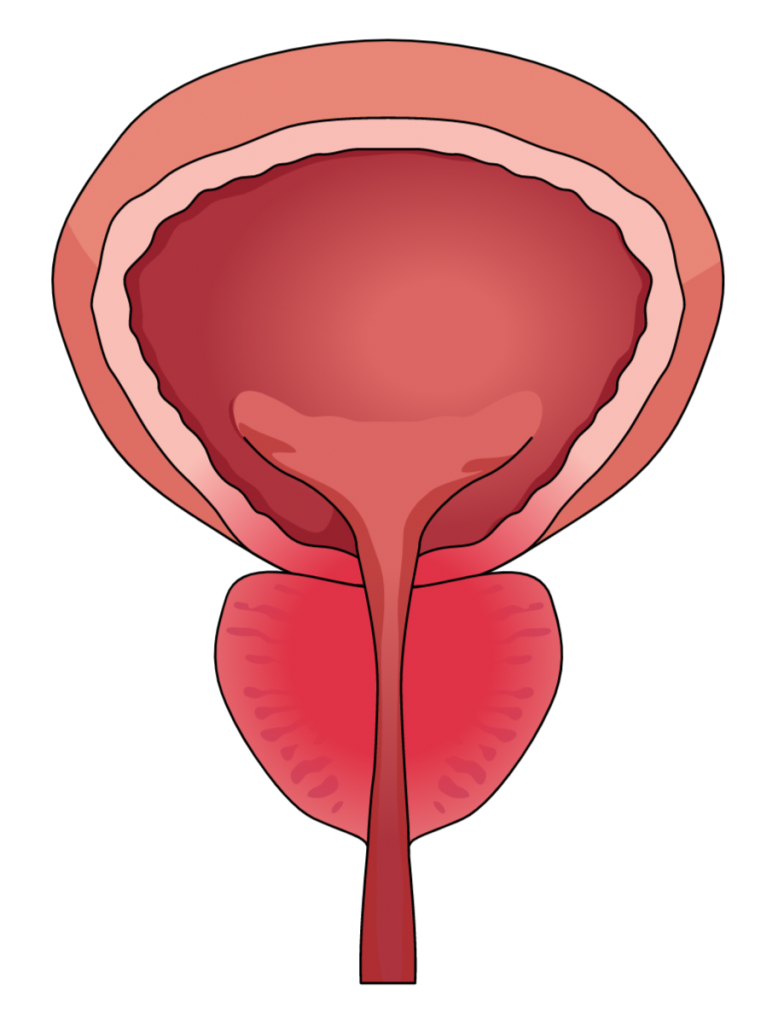
We already know that an inflamed prostate gland may affect the outer part of the rectum. Besides, between these two surfaces only a thin layer of fat is inserted. It is not a coincidence that in cases of bacterial infection, the bacteria detected belong to the Enterobacteriaceae family. The most common features of IBS that accompany inflammatory prostatitis are bloating and incomplete defecations. In addition, pain is regularly reported, more commonly at the lower part of the abdomen. Usually, colonoscopy or imaging techniques come out negative, whereas diverticula are a common finding. Like Nick, who was suffering from chronic prostatitis for 1 year before presenting with functional gastrointestinal symptoms.
Nick was a 45 years old bar manager with very vivid social and sexual life. At the age of 44, he started feeling a mild discomfort located at his genital. This symptom initially resolved by itself and Nick attributed it to his very intense sexual life. As time passed, however, the pain reappeared and became stronger. He was forced to get up to urinate several times during the night. In short, during the past year Nick visited 1 urologist, 2 gastroenterologists and 2 general practitioners, while he underwent colonoscopy, gastroscopy, ultrasounds, blood tests and several other laboratory tests, leading to no diagnosis.
Oral bacteria should never go past the stomach. This is why gastric acidity should be potent
Chronic inadequate fiber consumption, constipation and lack of physical activity inevitably lead to diverticulitis, even at younger age. SIBO also manifests early in life when diet and oral hygiene are not taken care
Prostatitis treatments are usually combinatory and long-term leading to the gradual damage of the commensal ecology
Repeated antibiotic treatment lead to the vicious cycle of IBS and prostatitis recurrence. Finally, systemic problems appear, like malnutrition and fatigue
Chronic periodontitis has constantly been supplying Nick’s large and small intestine with bacteria since the age of 25. This bacterial passage is normally terminated in the stomach. In Nick’s case, though, eating habits and heavy antibiotic use favored low stomach acid. In turn, low acidity favored gut enrichment with mouth and environmental bacteria. Besides, Nick’s diverticula are a very friendly place for bacterial overgrowth acting as sites of dysbiosis. The diagnostic panel was a large one due to all the comorbidities present and it included stool, blood and urine tests.
Bloating and gas are the opposite side of the same coin. Both rely on dysbiosis and the prevalence of fermentative gram-negative (mostly) bacteria)
The trapped air within the colon along with the loss of defecation timing leads to the constant feeling of colonic content and bowel movement
Suffering from both prostatitis and IBS can be very painful sometimes. The pelvic pain syndrome is very common in men with prostatitis
Mucus and water excretion is a defense mechanism in order to clear the colon from potential pathogens. This produces loose stool most of the times.
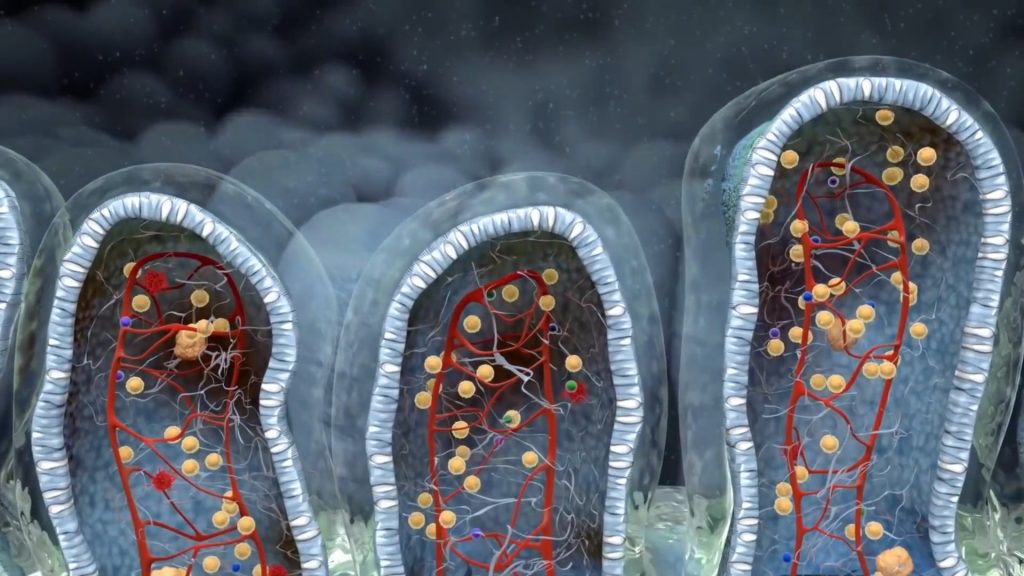
The results of Nick’s tests were indicative of a chronic inflammatory process. Inflammation was probably around the diverticula. As a consequence, it perturbed the mucosal environment permitting other pathogens to colonize. The pain he experienced was due to the infectious inflammation. In addition, this could explain the residual feeling he had after passing his stool. The microbial populations of Klebsiella and Veillonella are very common when the mucosal epithelium has lost its original physicochemical and immunological properties. This pathologic environment enables fermentative bacteria to produce air in a faster rate than the one it is evacuated. As a result intense and painful bloating appear.
Elevated sIgA
Elevated sIgA levels point to infectious inflammation. Symptoms associated with elevated sIgA are multiple defecations and loose stool

Elevated EPX levels
Elevated eosinophil activation leads to allergic symptoms, like itching and loose stool and in several cases produces the sensation of painful defecation
Klebsiella/Morganella overgrowth
Both these bacteria are potent fermenters of starch and histamine producers. Loose stool, itching and bloating are potent symptoms
Probiotic sterility
Probiotic sterility leads to abnormal fermentation of starch, sugars and fiber. Bloating and gas are main symptoms
Nick’s treatment consisted of three 1.5-month courses and three more meetings. The first stage of the treatment is the most risky. During this time, it is very important to avoid possible prostatitis recurrence as it will interfere with the treatment. For this reason, abstinence from any sexual activity is advised as well as the lifestyle choices that favor prostatitis – smoking, drinking, a sedentary life. John had no problem with the latter, and said that he would try with the former!

A few weeks later it was time to add a potent prebiotic formula. I told him to stop taking the extra antimicrobials but to continue with the potent one for 6 more weeks. I asked him to expand his night fasts to 5 days per week. That was not a problem as he had seen for himself the effect of this simple diet change. One and a half months later, he called me to report that he would not be able to visit me but everything was perfect. No bloating, no pain, and no diarrhea.
Men with prostatitis may experience pain or discomfort in many areas of their pelvic region. Often this pain is a reflective one due to prostatic swelling and inflammation. Nevertheless, many studies have recently pinpointed the role of the gut microbiome in both the small and large intestine in the initiation, exacerbation and resolution of prostatitis. It seems that several microbial metabolites as well as the microbes themselves have the ability to migrate and infiltrate the prostatic tissues.
When a patient with past or current prostatitis asks for help with his gut symptoms, it is important to know that fixing just one of them is not an option. Prostatitis and IBS must be treated concurrently using multimodal approaches. John was a very successful case because he followed the program very accurately and he did not give up, despite the length of it.
- Prostatitis is a common finding in men suffering from irritable bowel syndrome and it provides useful information regarding the context of their gut symptoms
- Irritable bowel symptoms usually take 2 to 4 months to resolve and maintaining a gut friendly diet and lifestyle usually they never come back
- Bloating and residual feeling are the most prominent symptoms, whereas other symptoms like painful defecations and diarrhea are not uncommon
- The gut is interconnected both directly and indirectly with almost all other organs and thus a multidisciplinary approach is often required
- Lifestyle choices play a determining role for complete remission. Most important are smoking, dietary habits and sedentary life

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.