Post Infectious IBS
(A gut health story)
Post-infectious IBS (PI-IBS) refers to instances where symptoms arise following a viral or parasitic infection, most commonly gastroenteritis. This is Katie’s Post-Infectious IBS cure story
Number of cases
Mean age
Rate of success
Treatment duration
Most common symptom
Most common culprit
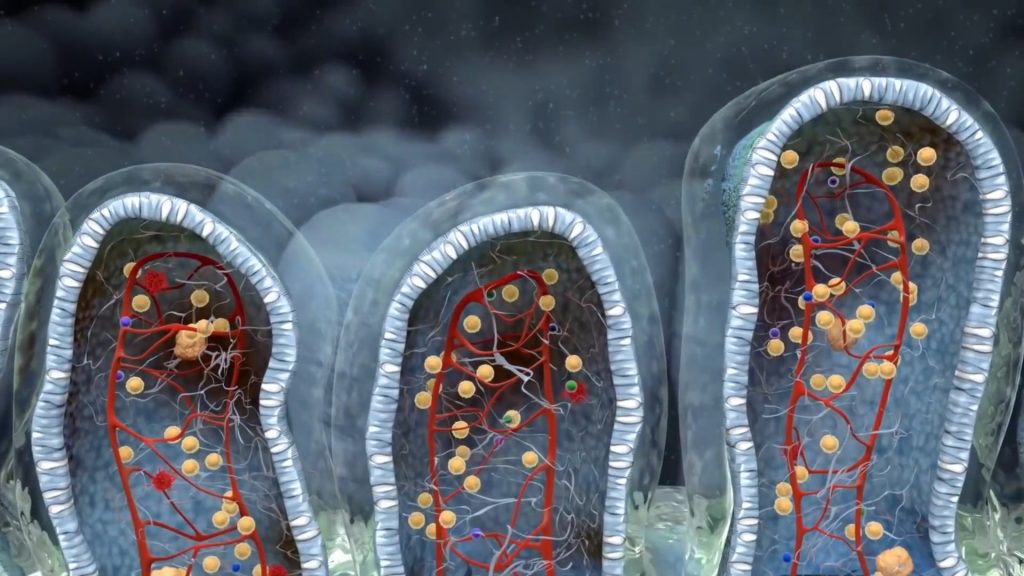
Most people suffering from any kind of irritable bowel syndrome, including the postinfectious subtype (PI-IBS), are usually predisposed to it due to various risk factors. Predisposition arises from a variety of factors, mainly nutritional, environmental, stressful, infectious, and some genetic. These people may be at the edge of manifesting IBS for years before symptoms, such as abdominal pain and changes in bowel habits, appear. The trigger that may bring their symptoms to the surface varies from case to case, with the most common being bacterial, viral, or parasitic infection. The intestinal mesh produced by the violent immune response against the infectious agent, such as bacterial gastroenteritis, sets the basis for the onset of the syndrome and increases the risk of developing PI-IBS.
It is the most common trigger of IBS. When the intestinal environment is already vulnerable due to inflammatory bowel issues, a powerful infectious agent may cause significant changes in both the mucosal layer and the microbial ecosystem, leading individuals to develop PI-IBS.
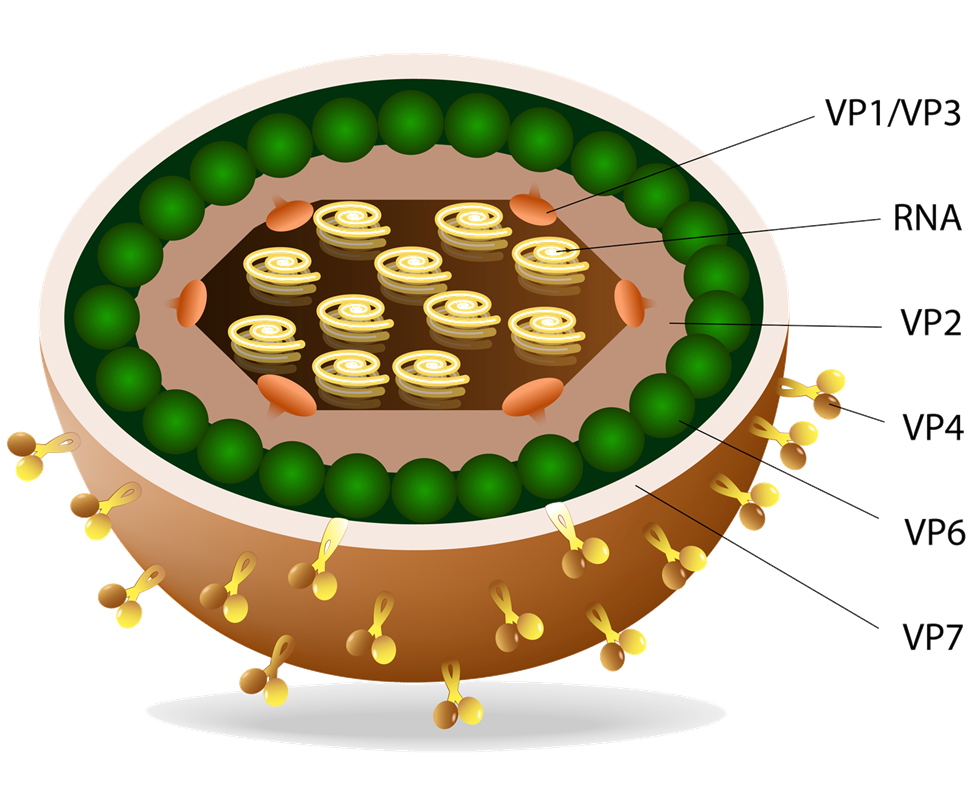
Other infections, beyond the gastrointestinal tract, significantly affect the immune response and tolerance of resident gut populations. These include infectious agents like HIV, CMV, Epstein-Barr virus, and many more.
The emergence of IBS after or during antibiotic treatment is very common. Most of the times the damage is reversible, it depends, however, on the chronicity of their use and the type of antimicrobial substances taken in the long run.
Radiation colitis is the most common complication of bowel and bladder cancer radiotherapy. In many cases, it is not possible to regain full intestinal function
Some surgical operations, mainly involving abdominal areas, may lead to the creation of scar tissue and the wrecking of local intestinal physiology. In addition, some reports blame anesthesia for inducing deleterious changes in the colon microbiome
Dental procedures are not rare triggers of IBS. Usually, this type of IBS resolves on its own.
There are several other triggers reported from patients, like during and after traveling by airplane, after visiting places with very high humidity, after moving to a new house, and more. Most of them eventually converge to one of the most common IBSyncrasies.
Katie was a perfectly healthy woman who until she turned 39 years old, had no symptoms of gastrointestinal origin. She reported that she would eat without any restrictions and never experience any problem. 2 years ago, after an evening scuba diving lesson, she returned home and, according to her report, she did not feel hungry as usual, so she just ate a yogurt. This was the last time she remembered being pain-free.
So, it begins
Several hours after eating the yogurt she started feeling an acute, strange pressure around her belly button and a few minutes later she ended up having watery and loose stools. This symptom pattern persisted for 6 days. Within the next year, she visited 3 MD’s, was prescribed various treatments, and underwent all kinds of tests, which all came back negative. Taking into consideration that her mother had passed from colorectal cancer, she could not help thinking of malignancy, although her colonoscopy was clear. The only thing that calmed her symptoms was loperamide (an anti-diarrhea agent), but she knew that this was just symptomatic relief.
Microbial perturbation early in life can alter the balance of the microbiome, paving the way for distorted mucosal properties and IBS. Early antimicrobial treatments play a major role in enhancing dysbiosis.
Inoculation of parasitic species. A well-nourished microflora can handle parasitic infections which usually present with mild gastroenteritis-like symptoms. However, a predisposed gut may suffer augmented damage, increasing the risk of developing PI-IBS.
Mold colonization. When the microbiome is already predisposed, mold can easily inhabit the gastrointestinal environment and multiply faster, giving rise to IBS symptomatology.
Chronic diarrhea. Parasites and bacteria that colonize the gut environment for longer than they should start secreting substances that condition the environment to favor their growth, instead of commensal bacterial growth, conferring higher risk for IBS onset.
The main aspects of Katie’s PI-IBS pathology that needed investigation were smelly gas, epigastric pain, diarrhea, and long-lasting burping incidents. All of them had a central cause, which was the deterioration of her microbiota (dysbiosis). Symptoms may, indeed, have been triggered by the spoiled yogurt she consumed, but the context this trigger took advantage of was the chronic dysbiosis attributed to the antibiotic abuse. Of course, I needed to exclude other, more serious non-IBS causes, like adult-onset celiac disease and sIgA deficiency.
The characteristic odor of gas produced by parasites or septic bacteria stems from sulfur and nitrogen conversion to hydrogen sulfide and ammonia, respectively
The episodic nature of loose or watery stool is usually attributed to the ever-changing microflora status
While burping is usually a stomach-derived symptom, in certain cases of IBS, gas may leak from the large intestine, especially when SIBO is present
Residual feeling is usually a false signal. That means that there is no residual fecal content inside the gut lumen; rather, the inflammatory reactions against the chronic agents, like Proteus, enhance the feeling of fecal material
This case is an excellent example of an IBS patient whose mainstream diagnostic tests are negative but a wealth of findings is revealed by advanced biochemical and molecular testing. In fact, the only negative result I got from Katie’s results was the blood celiac disease test. Heavy dysbiosis, inflammation, allergic mediators, malabsorption, and even a parasite had set the stage for Katie’s pathology, and it was not a simple one.
Histamine produces anaphylactic-like reactions in the gut leading to watery stool and other common IBS manifestations
D. fragilis (just like Campylobacter jejuni) is a constant eosinophil activator. EPX mediates allergic reactions both in the intestine and the circulation and is found elevated both in IBS and inflammatory bowel diseases
This bacterium produces hydrogen sulfide which makes gas smell. In addition, intermittent diarrhea and other digestive symptoms may be exaggerated by its presence
Katie’s treatment options were very limited due to the multitude of findings. For this reason, her treatment had several stages, each one aiming at different aspects of her syndrome, while implementing a medium-intensity low FODMAP diet. The first stage targeted the parasite along with gut and stomach lining protection. Once parasite levels were reduced, it was Proteus’ time. Due to the fact that I would use a specific treatment for D. fragilis, I chose a plant-based antimicrobial blend for Proteus, strong enough though. The last part of her treatment consisted of anti-inflammatory, anti-histamine, and gut-nourishing agents.

Two months later, Katie walked into my office obviously content with the course. She looked better as she regained the weight she had lost because of her bowel problem. Her diary was blank as her stools were now formed and gas was scarce, there was no burping after meals, and her psychology was very good. I told her to repeat the last two months and reassess several inflammation markers and a parasitology stool test.
Gastrointestinal issues have the potential to produce violent and long-lasting reactions. And Katie’s gut health story is just one example among hundreds. These violent responses are very important as they serve a lifesaving purpose: to inhibit the passage of microbes or toxins inside the body. Their impact on gut physiology is great, but a healthy gut microbial ecosystem can overcome this impact and restore proper digestion and a healthy intestinal tract.
Things get complicated in an already vulnerable gut
In a compromised ecosystem, imbalanced microflora and downregulated immune barriers (leaky gut) may not be able to overcome the issue, giving rise to long-lasting PI-IBS. While the case described above is a diarrhea-predominant one, many post-infection cases present with constipation.
Independently of the form the syndrome possesses, it is critical to identify the pathogenic bacteria overgrowth and the comorbid changes that have taken place because of the issue. This is why blood tests are not practical. Once this information is available, post-infectious IBS can be cured, and it usually is. The patients need to be insistent and not give up after the first flare-up. The agent that caused the issue in the first place is not to be blamed for PI-IBS; it is the imbalanced microflora and gut-associated immune barriers that cannot prevent the outcome.
Katie's Post Infectious IBS cure story
- Infections may trigger IBS, but in order to do so, other predispositions must exist. Heavy dysbiosis or immune downregulation is the most common comorbidities
- Irritable bowel symptoms usually take 2 to 3 months to resolve but a strong immune-enhancing treatment must be followed for at least 6 months
- While our gut ecosystem has an incredible capability of self-repairing, chronic assaults, like antibiotics and poor food choices may disrupt its balance
- Women are more prone to post infectious irritable bowel syndrome. It seems that some hormones make women more susceptible to dysbiosis

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.