IBS and diabetes
IBS and diabetes often go hand in hand. Patients presenting with both disorders usually present with limited exocrine pancreatic output and diarrhea. This is Michael’s real IBS story
Number of cases
Mean age
Rate of success
Treatment duration
Most common symptom
Most common culprit
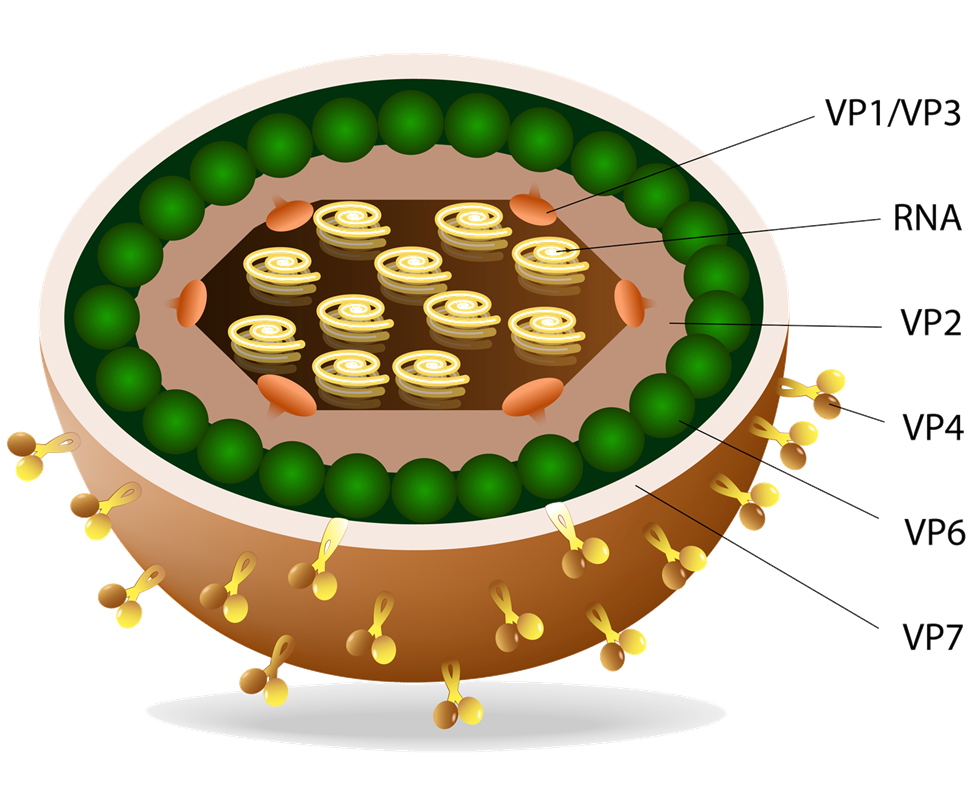
The process of metabolizing food, particularly from animal sources, hinges significantly on the regulation of sugar and insulin. As we consume food, it undergoes preparation in our stomach before reaching our small intestine, where it interacts with various components, including pancreatic enzymes. These play a pivotal role in the complete breakdown of proteins, fats, and sugars. If these are not regulated properly, undigested particles move downstream, triggering unwanted effects such as bloat, diarrhea, and dysbiosis.
Gastrointestinal signs of exocrine pancreatic insufficiency
Often, but not always, imbalances like these present in the context of other conditions such as diabetes, chronic pancreatitis, bile obstruction, or post operations like gastric dissection. Because it’s thought to be a rare clinical occurrence, it often goes unnoticed. The primary issue here is that in many cases, these imbalances are at the root of gut issues, like IBS. Another problem is the common belief among many doctors and people with diabetes that imaging techniques like abdominal ultrasounds or CT scans can rule out any role of high blood sugar levels in their condition; this is not accurate. These techniques can only identify tissue changes, but they fall short in measuring the organ’s output. Consequently, these tests should be ordered whenever a patient reports symptoms such as diarrhea, abdominal pain, or constipation.
Currently, Michael is a 56-year-old individual responsible for maneuvering the public bus. For a decade and a half, his route has linked the maritime hub of Piraeus and Athens’ national airport. This assignment entails working in shifts, a routine that incorporates cycles of nocturnal duties every week. At the age of 49, he was identified as a patient with type 2 diabetes. Despite his attempts to manage his blood sugar levels through a controlled diet and regular physical activities, he initiated insulin therapy after a year. As symptoms like bowel irregularities and abdominal bloating surfaced, he failed to associate them with his diabetes condition. This was a common oversight among the half-dozen medical professionals he sought help from. His narrative aligns with that of numerous diabetic individuals who have assured me, “But my pancreas has been examined and everything appears normal.”
The timing of Michael's social activities (work, exercise, meals, socializing, etc) had a direct and profound effect on pancreatic function
Both the pathology of diabetes and insulin treatment confer a great impact on the development and maintenance of the gut microbiome
The ongoing loss of nutrients due to malabsorption creates a vicious cycle between exocrine insufficiency and IBS symptoms

In Michael’s case, diabetes, specifically type 2 diabetes mellitus, was a clear contributor to EPI, or exocrine pancreatic insufficiency. Yet, a handful of less significant potential causes combined might account for his full symptom profile. I hypothesized that the trio of major GI symptoms Michael identified—diarrhea with urgent bowel movements, bloat, and abdominal pain—were all secondary responses to EPI. This condition can cause food particles, mostly proteins, carbohydrates, and fats to decompose or undergo abnormal fermentation within the patient’s gastrointestinal tract, specifically the colon. This results in erratic, poorly distributed air production and continual water and mucus secretion from the intestinal walls.
Stool consistency is highly influenced by the proportions of nutrients (fat-soluble vs water-soluble) reaching the colon and the excreting capacity of the colon, at that specific time
Exocrine pancreatic insufficiency and the resulting enzyme inadequacy leads to defective food degradation. Indigested food particles may cause stomach and bowel cramps. both commonly manifesting as complications of diabetes
The bacterial fermentation of unabsorbed food, including fruits and vegetables is much more prominent in patients suffering from exocrine pancreatic insufficiency
While early satiety is one of the hallmark gastroparesis symptoms, it may also appear in the context of exocrine pancreatic insufficiency
Michael’s pancreatic elastase levels were virtually nonexistent, which not only led to diarrhea but also posed challenges in managing his type 2 diabetes. Moreover, a key bacterium known as Akkermansia, which is typically associated with maintaining stable blood sugar, was missing. Additional findings pointed towards a substantial depletion of probiotic cultures, the discovery of high-fat content in stool (indicative of steatorrhea), and detection of various fungi such as Geotrichum, known for its distinct lipase activity.
Actionable exam results (4 out of 8)
Akkermansia muciniphila deficiency
Akkermansia, besides being a commensal bacterium, is now considered a glucose homeostatic gut mechanism. In fact, it seems that metformin works only when Akkermansia is present
Exocrine pancreatic insufficiency
Diminished pancreatic output may explain all the patient’s symptoms, including malabsorption, urgency, diarrhea and even glucose fluctuations

Steatorrhea
Malabsorption of fat molecules may explain the fatigue, weight loss and floating droplets of oil on the toilet water
Probiotic sterility
Probiotic sterility leads to abnormal fermentation of starch, sugars and fiber. Bloating and gas are main symptoms
The plan I formulated for Michael targeted two critical areas: addressing exocrine pancreatic insufficiency and dysbiosis. The application of enzyme supplementation alone isn’t typically potent enough to accomplish total symptom abatement; the restoration of a patient’s social life is only actualized after the beneficial bacteria in the gut have been re-established. And that’s why the initial diet was a low fodmap one.
Merely depending on animal-derived enzymes will fall short, considering the severe depletion of Michael’s gut microflora. Such a condition wouldn’t permit him to digest plant-based fiber or complex carbohydrates efficiently. This situation becomes even more complex when we factor in the glucose levels in his body, which are inherently challenging to regulate due to his diabetes.
Undeniably, treating Irritable Bowel Syndrome (IBS) in patients who are also battling diabetes always necessitates an additional focus on their metabolic health. Instead, we hope to achieve a state of balance where the body can adequately manage its glucose, thus enhancing the overall health and well-being of individuals like Michael.

I reconnected with Michael after a span of six weeks. His ability to stabilize blood sugar had improved considerably, his digestive system functioned regularly, and his overall mood was upbeat. There were minor anomalies in his stool’s form and occasional bloating during this period, but he generally reported an 80% improvement in his health.
I assured him that these minor issues would dissipate gradually, possibly attributed to a ‘die-off’ effect. I urged him to adhere to a rigid 15:9 intermittent fasting routine and to strictly avoid alcohol. In addition, I told him to start adding more vegetables, outside the low-fodmap diet. We communicated again six months later. His condition was markedly stable, and he had effectively adjusted to the medication to the extent that his daily insulin dosage was reduced to 16 units, down from 24 units before starting the therapy.
Individuals with irritable bowel syndrome (IBS) who also exhibit signs of exocrine pancreatic insufficiency (EPI) are frequently left undiagnosed for extended periods. This often occurs because their symptoms are quickly categorized as “usual complications of their primary condition” – in this case, diabetes, and therefore, they go unaddressed. A common assertion they encounter is, “if we manage your diabetes, your gastrointestinal symptoms will dissipate”.
However, this isn’t entirely accurate – unless lipid absorption is reestablished, fluctuations in blood measurements become more frequent and more severe. It’s crucial for EPI patients to understand that complete pancreatic restoration may not be achievable. While I’ve observed modest to moderate improvement in some instances, it’s usually not substantial.
They need to be educated about meal planning and always bear in mind not to leave their digestive function unchecked. If they do, first EPI symptoms will reemerge, followed by a deterioration of their gut microflora, and eventually, malnutrition will set in.
- The gut health is directly and indirectly linked with nearly all other organs, necessitating often a multidisciplinary approach
- Diarrhea and feeling full after eating are the most common IBS symptoms within this context, while others like multiple defecations and weight loss are typical.
- Autoimmune disorders such as Type 1 diabetes, psoriasis, celiac disease, and spondyloarthropathies can cause exocrine pancreatic insufficiency. Likewise, surgeries including cholecystectomy, gastrectomy, and colectomy may bring similar complications.
- Diabetes, along with other metabolic disorders, are tied to digestive system challenges, leading to complications that mimic those of diabetes and irritable bowel syndrome, even without diabetes being present.
- Lifestyle choices hold the key to complete remission. Crucial are regular fasting periods, adherence to natural circadian rhythms (sleep, training), and a diet promoting gut health.

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.