Crohn’s after visiting tropical country
36 y.o male whose Crohn's disease appeared a few days after a trip to Colombia
Everyone’s microbiome has been shaped by several factors. Starting from our mother’s vaginal microbiome during birth to the amount of antibiotics we have consumed throughout our life, the microbiome is constantly changing. One factor that makes the microbiome of a specific population being kind of similar is geographic location and the culinary habits of a nation. In this context, Japanese have a completely different microbiome than Mexicans do. And while raw fish is very common in Japan, a Mexican will probably experience gastrointestinal disturbances after that sushi. In several cases, a sudden shift in the diet of a person could produce massive changes in his microbiome, even bring into surface a predisposition for autoimmunity.
Gaulke, Christopher A., and Thomas J. Sharpton. “The influence of ethnicity and geography on human gut microbiome composition.” Nature medicine 24.10 (2018): 1495-1496.
Rehman, Ateequr, et al. “Geographical patterns of the standing and active human gut microbiome in health and IBD.” Gut 65.2 (2016): 238-248.
Jim C. was a perfectly healthy 36 years old swimmer who had never experienced any gastrointestinal symptoms. From his medical history, the only time his stomach bothered him was during a gastroenteritis when he was 9 years old. That’s all he could remember. He loved surfing and travellling around the world. His last trip was in Colombia. Before traveling he got the recommended yellow fever vaccine. He did not report any side effects from the vaccine. 15 days later he returned from Colombia and the only incident he can remember is being bitten by several mosquitos during an inland excursion. A few days later he noticed his lower abdomen swelling, but the swellling was constantly moving, until his testicles got swelled as well. The swelling insisted for about a week and then resolved on its own.
The only thing that led Jim to visit a doctor was the slight change in stool shape. The gastroenterologist performed several blood tests and noted an elevation in CRP value, which was reproduced 10 days later. Then he ordered a calprotectin test (880) with the result indicating massive leukocyte activation. The diagnosis was ultimately confirmed afte the colonoscopy, which revealed a Crohn’s disease image that certainly did not match the lack of GI symtpoms. He started prednisone and mesalasine and two months later he came to see me in my office.
The course of the treatment could not be monitored since Jim had no symptoms at all. This is rare but I have seen it before. Jim had just finished his first treatment and was asked to repeat calprotectin. The value was much better but not normal (336). I decided to take it a step forward.

Jim had been exposed to a completely different diet during his trip to Colombia. Maybe this is not enough to bring into surface an autoimmune disorder, but in an already predisposed person, genetically or environmentally, such a violent microbiome rearrangement could do the job.
Parasitic infections may mimic IBD both clinically and diagnostically
The sudden urge to defecate may be a symptom of IBD, but also of a potent parasitic infection
The immune augmentation in order to fight a parasitic infection is extremely energy-consuming
Mucus is the first line of gastrointestinal passive defense and increases during an active infection
Mohammadi, Rasoul, et al. “The relationship between intestinal parasites and some immune-mediated intestinal conditions.” Gastroenterology and hepatology from bed to bench 8.2 (2015): 123.
The probiotic sterility was pronounced, and so was the other two inflammation markers, besides calprotectin (EPX and sIgA). The most prominent, though, finding was too many Blastocystis hominis full parasites as well as trophozoites. In addition, several strains of Citrobacter were recovered in vast amounts.
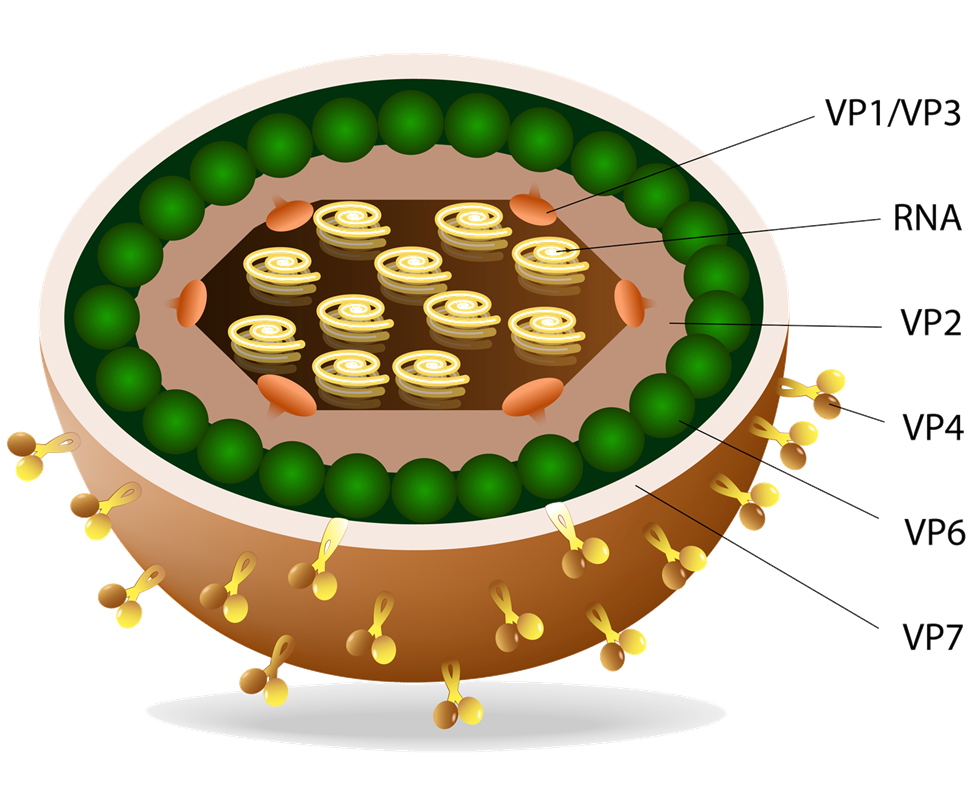
Blastocystis hominis
Parasites like Blastocystis have long been suspected to be involved in the pathogenesis of inflammatory bowel diseases
Elevated sIgA
Elevated immunoglobulin A is indicative of a chronic infectious inflammatory reaction. Serum IgA was within normal range
Citrobacter spc
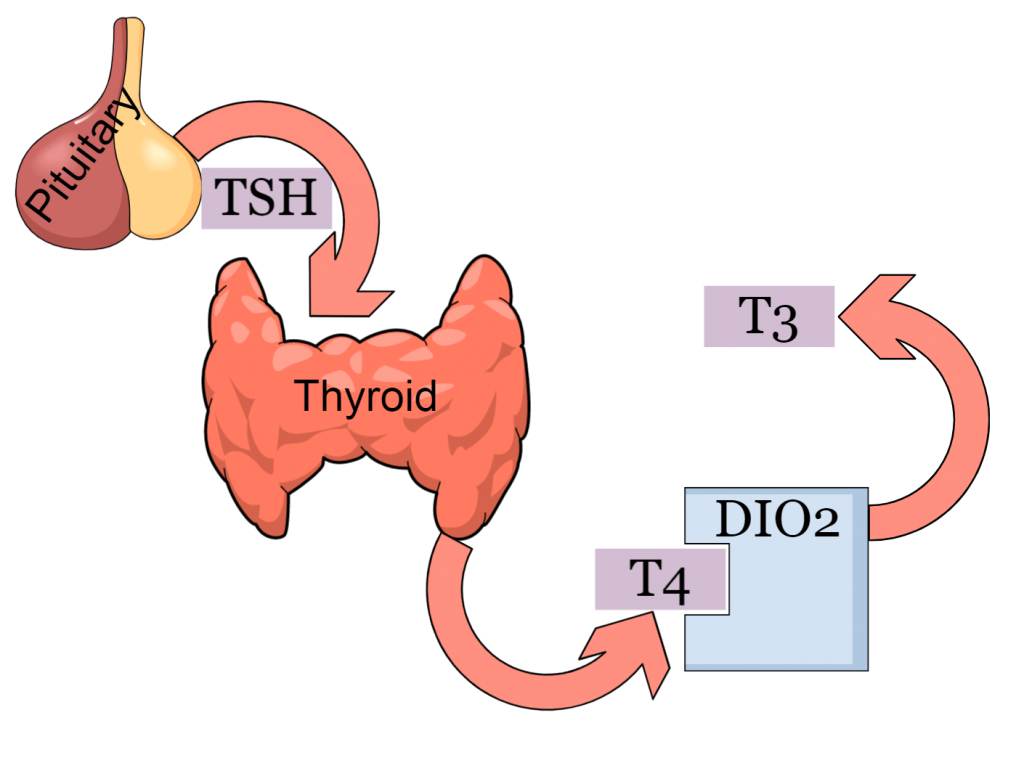
Vitamin D deficiency
Vitamin D is crucial in all autoimmune disorders, including Crohn’s colitis
EPX
This is a very sensitive eosinophil activation biomarker.
Parasites are hard to eliminate. Despite the mainstream view, protozoa like B. hominis can’t get eliminated using just metronidazole. Nevertheless, a 10-day antiparasitic course, repeated 3 times during a 3-month time window will certainly be more effective, under the condition that all other aspects of the disease are equally covered. In this case, the presence of too many gram-negative bacilli (Citrobacter) dictated simultaneous antibiotic treatment, at least during the first metronidazole treatment. A third pharmaceutical, appropriate in this case is budesonide. The large amount of activated eosinophils, probably due to the parasitic overabundance, should be quenched.

In Jim’s case, it was first provided after the first month of antibiotic treatment, and indeed, that is when he felt much better, his urgency episodes disappeared and his stool were completely formed. Finally, a large dose of vitamin D was given, until his serum value reached above 60 (63,3). Jim was able to discontinue prednisone without relapse and stay on mesalazine and an intermittent schedule of budesonide (twice per year for 2 months). His last colonoscopy was clear, without any sign of a relapse and he experiences less fatigue.
- Parasites are recovered more often in IBD patients, but whether they play significant role in disease progress is not clear
- Patients usually feel better after metronidazole treatment but other aspects of the infestation should be taken into consideration, like eosinophilic activation
- Travelling to countries with totally different culinary culture should be taken into consideration by people with history of autoimmunity or at great risk of IBD
- Gastrointestinal symptoms after trips to tropical countries should be addressed as soon as possible
- This is another example that reinforces the notion that IBD always manifest in the context of a gut dysbiotic state

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.