IBS and chronic mesenteric ischemia
72 y.o lady whose symptoms start right after her meals and last for 1-2 hours

The symptoms of irritable bowel are heterogeneous and often overlap, making them very difficult to attribute them to a specific cause. Small details, however, can point to specific causes. One of these details is the time after the meal when the symptoms start. Based on the perfusion course of the various organs during digestion, the possible number of diagnoses can be limited and a more targeted diagnostic approach can be made.
The first meeting was with the patient’s daughter. Her mother, Melina, was pretty tired of looking into her symptomatology. During the last 3 years she had visited too many doctors and had performed dozens of medical tests. None of these revealed something clinically relevant, and every therapy she had been on seemed to help her only for a while. Melina was a retired teacher. She was generally an active person throughout her life taking care of her diet while she was exercising almost daily. Nevertheless, abuses were not missing. The most important of these was smoking, a habit she had stopped for over a year now, but she had overall smoked for more than 45 years. She had not experienced any gastrointestinal disturbances, except a brief constipation period, right after menopause. Her main problem appeared three years ago.
At first she thought she had an age-related metabolic problem, but as time went by, she was able to clearly distinguish the pattern of the her symptoms. 20-30 minutes after eating a meal, a low abdominal pain started, presenting constant fluctuations for 2 to 3 hours and then spontaneously disappeared. At the same time, she noticed that, for no reason, she suffered from moderate to severe nausea. Over the last 3 years, she had visited all the possible specialties and had done all possible exams. The only positive findings were an increased serum homocysteine value, poor lipidemic control, and some stomach irritations after her last gastroscopy. The final diagnosis for her symptoms was … stress !!! Mrs. Melina had lost enough weight as she avoided meals in order to avoid pain.

After eating a medium meal blood perfusion is becoming gradaully more intense. 20 minutes after meals the vessels that supply blood to the large intestine are in full effect
Since the problem is blood flow, once the digestive phase is finished, blood is withdrawn and the symptom disappears
People with chronic mesenteric ischemia may experience weight loss, abdominal pain after eating, nausea, diarrhea, or vomiting
After years of pain conditioning, food avoidance leads to weight loss
After the narrowing of the vessels becomes very extended, symptoms may appear even in the absense of digestion
Previous diagnostic procedures had already excluded tumors or autoimmune inflammatory processes. In this regard, the stenosis of 2 vessels found in CT angiography set the basis for the diagnosis. Chronic mesenteric ischemia is diagnosed when all other possible causes have been excluded. The resulting preference for blood flow to the stomach is the large reduction in small intestinal motility and absorption. This is the reason why when the meal passes through the small intestine (needing much more blood) pain and inflammation appear. In Melina’s case, the fact that the pain was present even without eating is suggestive of an increased chance of a cardiovascular event occurring in the near future.
In the same time, high Candida concentrations and increased intestinal permeability were detected. Probably an accidental finding was also the very low pancreatic elastase, either due to age-related degeneration or due to hypoperfusion. Obviously, our first action was to inform her surgeon who immediately planned the stent operation. The rest would be treated afterwards.
Candida albicans
Elevated yeast levels indicate deteriorated mucosal properties
Exocrine pancreatic insufficiency
Low levels of exocrine pancreatic output could be attributed to age or abuses
Increased intestinal permeability
Chronic ischemia leads to disrupted intestinal barrier, permitting in this way mycotoxins to enter the circulation and pancreatic enzymes to act on the intestinal wall
Probiotic sterility
Not a sign of Lactobaciili or Bifidobacteria on stool
Stenosis affecting 2 vessels
Chronic smoking induced the stenosis of 2 vessels which supplied blood to the small intestine. The reduced blood supply during the blood demanding intestinal phase led to pain after meals
Melina finally came to my office 1,5 month after the operation. She reported that the pain had already diminished drastically whereas nausea had disappeared. Additionally, she had gained 1,5 kg and her appetite was back. Althoug new symptoms had emerged, like bloating and 1-2 diarrheas she did not seem concerned about them. Besides, we already how to deal with these symptoms.

Melina was now the most obedient patient and it took about 2 months to get into full remission. Her nutrition and exercise schedule was very strict and she agreed to go into an intermittent fasting plan soon after she returned to her normal weight.
- Patients over 60 (mostly women) already predisposed for cardiovascular disorders must be checked for chronic intestinal ischemia as soon as post meal symptoms appear
- Less common symptoms of chronic mesenteric ischemia are nausea, anorexia and diarrhea
- When pain appears in the absence of meal consumption, the manifestation of a cardiovascular event within the next 6-12 months is very probable
- Some comorbidities of chronic mesenteric ischemia are pancreatitis, inflammatory bowel diseases and gastric or duodenal ulcers
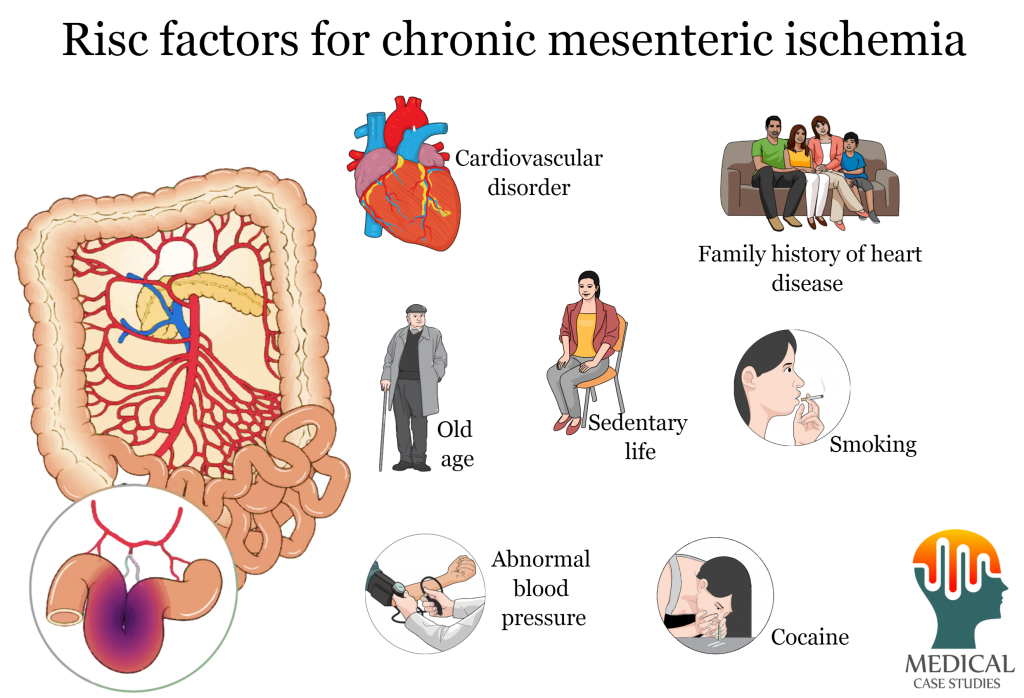
- Smoking, sedentary lifestyle, family history of cardiovascular disorders, personal history of CVD and cocaine abuse are predisposing factors for chronic intestinal ischemia

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.


