Pseudomonas-predominant IBS
Patients who suffer from IBS mimicking celiac disease and whose MS-microbiology tests reveal massive colonization by Pseudomonas spc
Number of cases
Mean age
Rate of success
Treatment duration
Most common symptom
Most common culprit
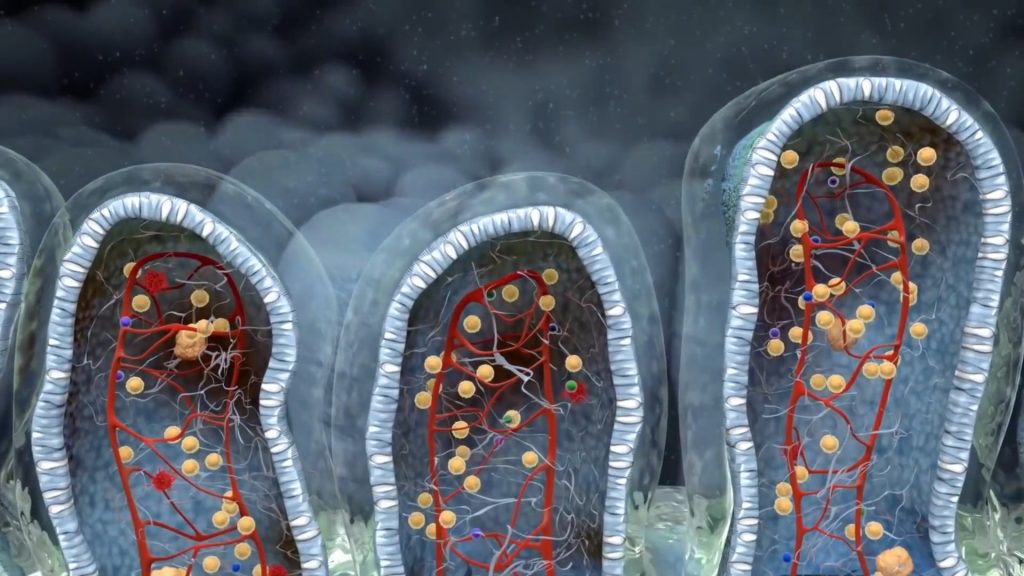
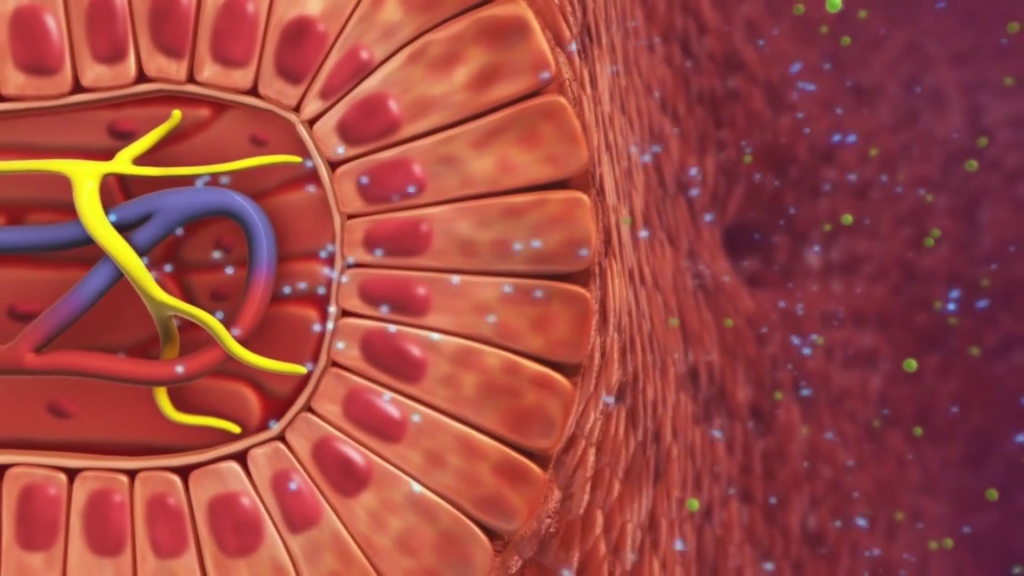
Normally, when assessing the human gut microbiome we mean the large intestinal one. There are, though, some bacteria that may produce IBS-like symptoms when they colonize the duodenum (small intestine). Pseudomonas aeruginosa is one of them. Microbiological assessment of duodenal biopsies reveal P. aeruginosa is not an infrequent finding in mixed IBS patients. The main biochemical property that makes P. aeruginosa notorious is the elastase activity, which permits it of breaking down gluten into highly antigenic fractions. These in turn mimic celiac-like antigens and produce a constant, low grade inflammation, in the absence of any celiac disease biomarker.
Does this mean that P. aeruginosa causes celiac disease?
Of course not. But it can make the gluten molecule equivalently antigenic and thus, produce the same symptoms, as celiac disease does. Celiac disease is the inability of proper gluten breakdown, which leaves gluten particles in a form that makes our immune system attack them. This makes our small intestine to be inflamed for several hours after the ingestion of gluten containing foods. P. aeruginosa, on the other hand, when inhabiting the duodenum, is one of the first population that comes in contact with the freshly consumed gluten. The special elastase enzyme binds gluten, and breaks it down is such a way that our immune system does not recognize the particles. Inevitably, the same inflammatory cascade that we find in celiac patients is commenced.
Aspa is a 56 years old mother of two, both delivered via C-section. While she was pregnant she gained over 20 kg. She was born in a small village in Greece and as a child she had recurrent tonsillitis episodes which led her to receive over 30 prescriptions of antibiotics until the age of 12. Even now she can remember that she already had several abdominal symptoms, mainly bloating and gas, and as a teenager she was always constipated. However, until 2 years ago her abdominal discomfort symptoms were intermittent so she did not pay much attention to them.
Pets carry many bacteria in their skin and their saliva without presenting any illness. These bacteria may inoculate a vulnerable human intestine and exert their metabolic functions
Pseudomonas aeruginosa is a bacterium that takes advantage of the low gastric acidity induced by PPI medicines and passes to the small intestine where it thrives
The chronic low grade inflammation produced by gluten elastase favors further Pseudomonas expansion and small intestinal permeability
Constant low inflammation along with enhanced Pseudomonas metabolism shifts mucosal properties towards a more pathogenic profile giving rise to IBS symptoms

The diagnostic panel I asked Aspa to perform was intended to assess mainly my suspicion of a small intestinal pathogenic event, rather than the usual colon dysbiosis. Besides the full 16SRNA stool test, I asked to perform several inflammatory biomarkers, both in stool and in serum. Additionally, a histamine work-up to exclude is useful in similar cases in order to exclude histamine intolerance. Fianlly, I wanted to check if she suffered from protein malabsorption (very common in small intestinal enteropathies) and pancreatic insufficiency.
The involvement of the upper small bowel in this IBSyncrasy, besides classic IBS symtpoms produces stomach symptoms soon after meals.
The potent gliadin elastase activity of this bacterium makes the consumption of gluten-containing foods problematic
Besides elastase, Pseudomonas possesses other metabolic activities which give as gas as end metabolic product. Most commonly, ammonia and methane.
Inflammation, malabsorption and limiting food intake provoke malnutrition and fatigue
Indeed, P. aeruginosa was recovered and the extent of colonization was >25 times the baseline reading. This means that statistically there were several billion P. aeruginosa cells, using their elastase activity to produce antigenic gluten fragments. These, in turn provoke a constant low-grade inflammation. In addition, at least 3 more results indicating malabsorption and low-grade chronic inflammation were recovered.
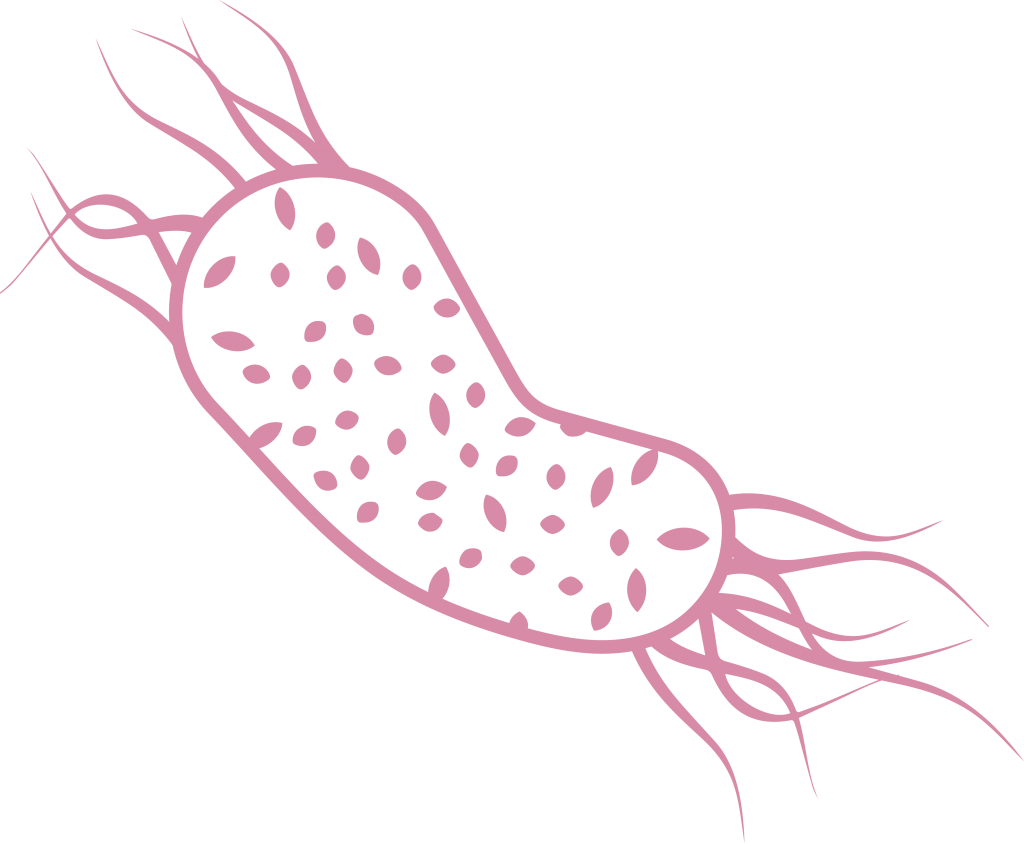
Pseudomonas aeruginosa
Low grade inflammation, burping and gluten sensitivity are the hallmarks of duodenal and jujenal colonization of this bacterium
Elevated EPX levels
Elevated eosinophil activation leads to allergic symptoms and reactions against food
Elevated sIgA
Elevated sIgA levels point to infectious inflammation
Probiotic sterility
Probiotic sterility leads to abnormal fermentation of starch, sugars and fiber. Bloating and gas are main symptoms
The basic principle for restoring small intestinal function is dual. It includes the depletion of harmful bacteria, like P. aeruginosa and the restoration of the damage that’s been already done, due to the chronic low-intensity inflammation. Very importantly, the antimicrobial agents administered should be followed by a 16-hour fasting. The concept behind this time restriction is that the small intestine must be in a restful state in order to heal. This may produce some extra bloating and discomfort in the first days of the treatment, but as the bacterial populations gradually decline, the symptoms will lessen. The treatment schedule was divided in two parts.

Our next conversation took place in a very pleasant atmosphere. She had experienced only one urgent movement in the past five days and her bloating had almost vanished. She had also tried a raw salad with very little discomfort after it. Two months after she started the treatment she was obviously a lot happier. She reported that three weeks had passed with regular motions without urgency and minimal gas production. She had already incorporated a lot of different meals on a daily basis and her increased energy was obvious to everybody.
Small intestinal bacterial overgrowth is a well recognized entity despite the difficulty in diagnosing it. The breath test is not very accurate as it can be compromised by several gastric factors and depends heavily on the patients previous meals. Nevertheless, overgrowth of several bacteria has been demonstrated to disorganize the small intestinal mucosal surface and to produce many unpleasant symptoms which, sometimes, may end up producing malabsorption and malnutrition.
- Pseudomonas aeruginosa may inhabit the small intestine and produce celiac disease-like symptoms in absence of celiac disease
- A specialized elastase enzyme Pseudomonas possesses has the ability to degrade in an immunogenic way gluten particles
- Most of the patients whose small intestine has been inhabited by Pseudomonas are pet owners. Pets may suffer from Pseudomonas-originated otitis media without obvious symptoms
- The timing of the treatment is crucial when it comes to small intestinal damages
- Use of proton pump inhibitors facilitates the passage of Pseudomonas into the small intestine, as it reduces the acidity of the stomach that would have kill it in the first place

With a background in Chemistry and Biochemistry from the National and Kapodistrian University of Athens, Theodoros brings a wealth of knowledge in functional medicine and advanced treatments to his role. He possesses exceptional skills in analysis, pattern recognition, diagnostic translation, and storytelling. He is also FMU certified in Functional Medicine and has received training in advanced treatments from the Saisei Mirai Clinic in Japan.